Oral Oncol:口腔HPV感染可致头颈癌
2015-03-02 MedSci MedSci原创
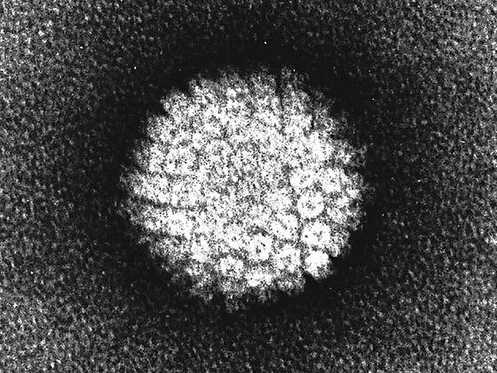
Oral Oncol:口腔HPV感染可致头颈癌关键词:头颈癌 HPV 口咽癌引言目前全世界最常见的病毒感染史人乳头瘤病毒(HPV)感染,感染了至少6亿3千万人。HPV至少有150种不同的病毒株,其中一些是致癌的(HPV16和HPV18),可能与生殖器癌和口腔癌有关。首次提出HPV与口咽癌相关是在30年前,HPV不再认为是口咽癌的危险因素而是口咽癌的发病因素。在发达国家,包括美国,HPV至少和90%
目前全世界最常见的病毒感染史人乳头瘤病毒(HPV)感染,感染了至少6亿3千万人。HPV至少有150种不同的病毒株,其中一些是致癌的(HPV16和HPV18),可能与生殖器癌和口腔癌有关。首次提出HPV与口咽癌相关是在30年前,HPV不再认为是口咽癌的危险因素而是口咽癌的发病因素。在发达国家,包括美国,HPV至少和90%以上的口咽癌相关。据统计,在美国,大多数性行为活跃的成年人在其一生中都会感染HPV。
通常认为头颈癌(HNC)与吸烟喝酒有关,高达75%的头颈癌病例与这些因素有关。然而,研究表明,吸烟喝酒所致的头颈癌正在减少,而HPV相关性头颈癌,特别是口咽癌,正在增加。实际上,1980s以来HPV阴性的头颈癌(与吸烟喝酒有关)其发病率下降了50%,而HPV阳性的头颈癌其发病率增加了225%。与烟草所致的HNCs(主要发生在60岁以上人群)不同,口咽癌好发在60岁以下的人群而且很多病例显示这些患者无吸烟喝酒史。
HPV相关性口咽癌的主要危险因素是口腔HPV感染,口腔HPV感染主要是通过性传播,相关的性行为包括早期性交、多性伴侣、口交以及舌吻(HPV感染发生率相对较小)。文献记载的其他的危险行为还包括性别和吸烟等。男性患HPV相关性口咽癌的患病率约为女性的二倍,吸烟可能会增加患口咽癌的几率,因为香烟中含有诱变剂和致癌物。目前正在使用HPV疫苗来预防HPV病毒株,尤其是HPV16和HPV18,引起的头颈、肛门和生殖器癌。几乎所有的头颈癌都能发现HPV16和HPV18,尤其是HPV16。
尽管HPV疫苗并未推荐用来预防口腔HPV感染,哥斯达黎加的一个临床试验表明HPV疫苗在预防HPV16和HPV18感染100%有效。然而,面对着HPV阳性的口腔癌发病率不断升高,HPV疫苗接种率仍然不理想。其中一个原因是由于对HPV疫苗,HPV以及HPV与头颈癌的关系了解甚少。唯一的一个已知研究是在美国东南部女性为主的白种人中调查了当地人对于HPV与HNC关系的了解。然而,相比于女性,口腔HPV感染与口咽癌在男性则更为普遍。
本研究的目的是为了评估人群对HPV疫苗、HPV和HPV与HNC的了解水平,以及这些知识水平与性行为习惯、危险性行为、和以男性为主的非洲裔美国人群的风险认知之间的关系。本研究也对目标人群HPV感染来源进行了表征。本研究的样本大部分是非洲裔美国人,相比于白种人,其头颈癌死亡的危险性较高。
摘要
目的:为了了解HPV,以及HPV与头颈癌(HNC)的关系以及高危人群对HPV的认识。
材料和方法:横断面调查2013年东圣路易斯飙车人员。
结果:只有29.9%的人知道HPV会增加患HNC的风险,42.4%的人认为HPV与HIV一样,只有25.1%的人从保健医师那了解过HPV。认为性伴侣数目没有增加患HPV的风险的研究对象对HPV的了解得分较低(r=0.74,p<0.001)。这与对HNC知识、性伴侣数目、初次性交年龄以及对危险因素的了解之间具有显著地关系;那些认为性伴侣数目多不会增加HPV感染几率的人员得分较低的概率增加33倍(OR=33.27;95% cl:16.34,64.74)。
结论:对HPV以及HPV与HNC的关系的了解在这一人群中具有显著地差异。
原始出处:
Osazuwa-Peters N, Wang DD, Namin A, Vivek J, O'Neill M, Patel PV, Varvares MA.Sexual behavior, HPV knowledge, and association with head and neck cancer among a high-risk group.Oral Oncol. 2015 Feb 12. pii: S1368-8375(15)00023-8. doi: 10.1016/j.oraloncology.2015.01.011.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











好文章,还会关注
83
#Oncol#
41
很不错学习了
142
#Oral#
38
#头颈癌#
40
#HPV感染#
44
洁身自好最安全
81