Dig Dis Sci:酒精性急性胰腺炎患者30天内再入院率明显较高
2021-12-24 MedSci原创 MedSci原创
酒精所致胰腺炎—alcholic pancreatitis 与有害饮酒相关,以胰腺的炎症、坏死为特征的病变,多伴有纤维化和功能异常,起病和病程可急,也可慢。
酗酒是全世界导致相关死亡的主要原因之一,饮酒导致每年超过 100,000 人死亡。酒精会影响身体的每个器官,它是急性和慢性胰腺炎的最常见原因之一。急性胰腺炎 (AP) 有多种病因,但其中最常见的是胆源性胰腺炎和酒精性急性胰腺炎 (AAP)。AP 的发病率为每 100,000 人中 8 至 50 人,死亡率高达 30% 至 50%。利用 2013 年国家再入院数据库 (NRD),25.7% 出院诊断为 AP 的患者会继发AAP。在这项研究中,13.7% 的 AP 患者在出院后 30 天内再次入院。本项研究旨在探究酒精性急性胰腺炎 (AAP)患者 30 天再入院率、原因和再入院预测因素。

为此,研究人员使用医疗保健研究和质量机构的 2016 年医疗保健成本项目 NRD 进行了一项回顾性队列研究。NRD 包含大约 1500 万份住院患者出院记录和 100 多个临床和非临床数据元素。主要结果是 30 天的全因医院再入院。次要结果是:指数入院和再入院的院内死亡率、再入院期间医疗保健相关资源的利用,包括:住院时间 (LOS)、总住院费用和成本,以及再入院的独立危险因素。

研究人员对 2016 年国家再入院数据库中因AAP入院后 30 天内再入院的成年患者进行回顾性分析后发现,2016年共有76,609例AAP患者出院,30天再入院率为12%。再入院的主要原因是 AAP。再入院与更高的死亡率(1.3% VS 1.2%;P = 0.21)或住院时间延长(5.2 VS 5.0 天;P = 0.06)无关。总的医疗保健经济负担为 3.54 亿美元。再入院的独立预测因素是有医疗补助保险、Charlson 合并症指数≥3、使用全肠外营养、阿片类药物滥用障碍、既往胰腺囊肿、慢性酒精性胰腺炎和其他慢性胰腺炎。肥胖与较低的再入院几率有关。
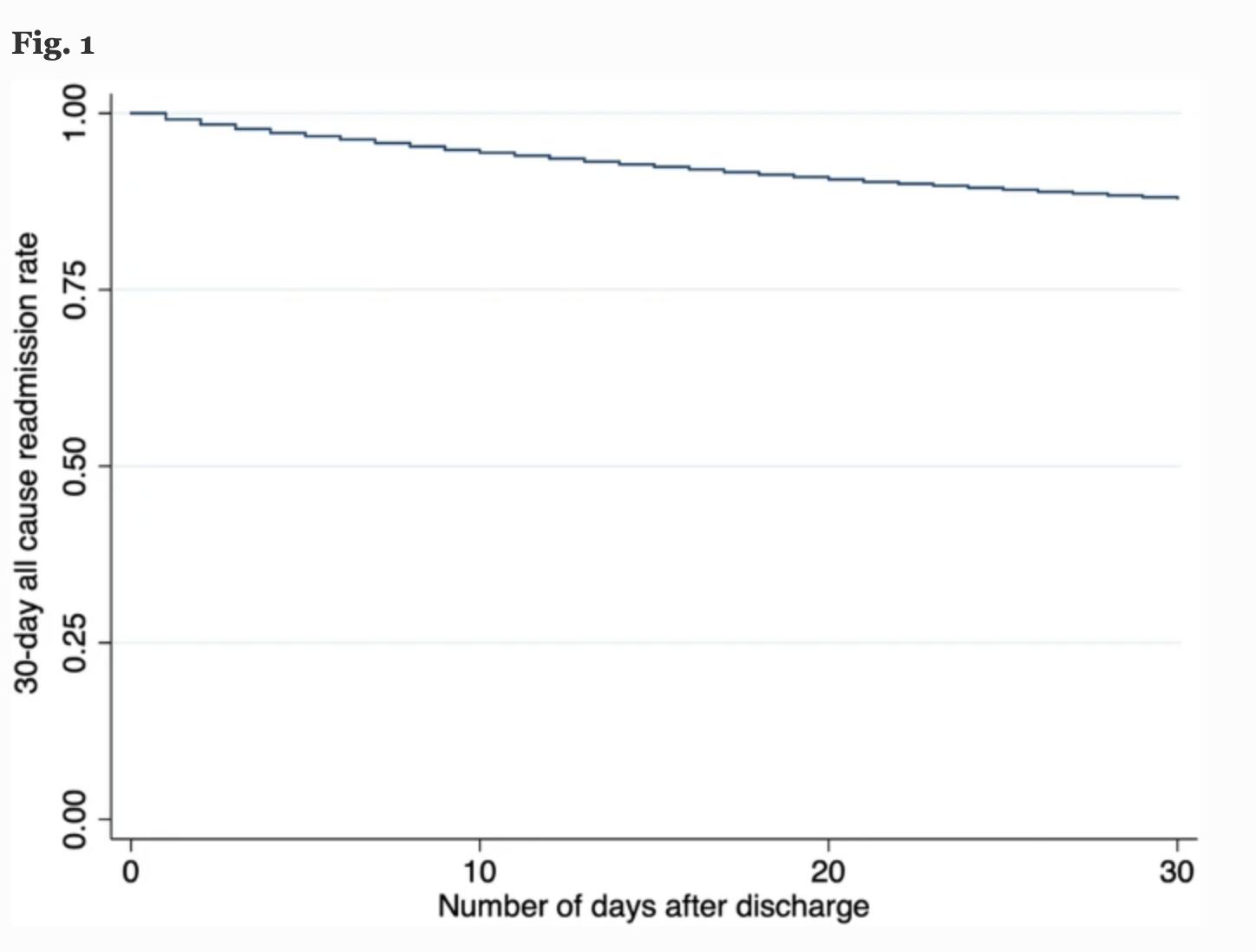
本项研究证实AAP 的再入院率很高,其主要原因是 AAP 的反复发作。酒精和药物滥用给我们的医疗保健系统带来了沉重的负担。公共卫生战略的目标应该是提供酒精滥用障碍康复和戒烟资源,以减轻再入院、医疗保健系统的负担并改善患者的预后。
原始出处:
Pedro Palacios Argueta. Et al. Thirty-Day Readmission Among Patients with Alcoholic Acute Pancreatitis. Digestive Diseases and Sciences.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#30天#
49
#Dis#
38
#酒精性#
30
学习了
59
#再入院率#
52