Nature:详解FDA批准的45款肿瘤靶向药物(名称、适应症、靶点、副反应、价格&注意事项)
2016-12-30 佚名 生物探索
Nature Review近期发表文章,盘点了迄今为止所有获FDA批准的抗肿瘤靶向药,并详细介绍了它们的名称、适应症、靶点、一般副反应、严重副反应和价格&注意事项。 所谓癌症分子靶向治疗(Molecular targeted cancer therapy,TCT),是在细胞分子水平上,针对已经明确的致癌位点(该位点可以是肿瘤细胞内部的一个蛋白分子,也可以是一个基因片段),来设计相应的
Nature Review近期发表文章,盘点了迄今为止所有获FDA批准的抗肿瘤靶向药,并详细介绍了它们的名称、适应症、靶点、一般副反应、严重副反应和价格&注意事项。
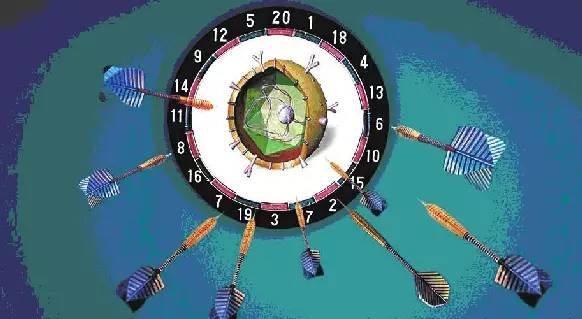
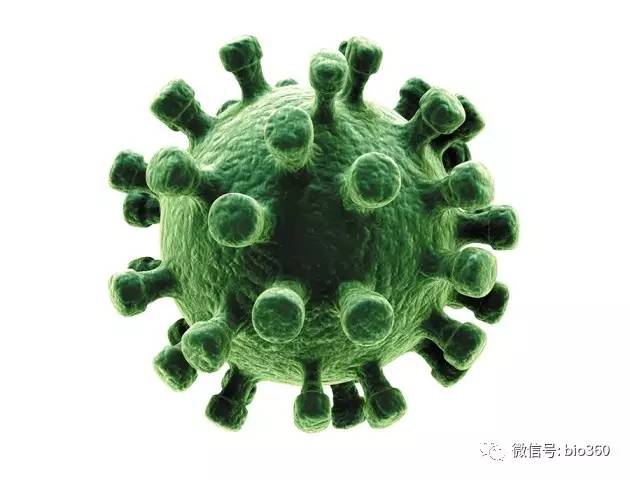
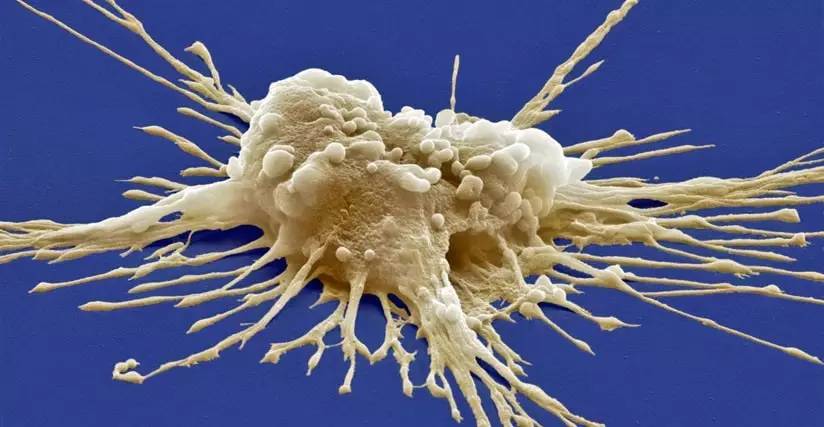
所谓癌症分子靶向治疗(Molecular targeted cancer therapy,TCT),是在细胞分子水平上,针对已经明确的致癌位点(该位点可以是肿瘤细胞内部的一个蛋白分子,也可以是一个基因片段),来设计相应的治疗药物,药物进入体内会特异地选择致癌位点来相结合发生作用,使肿瘤细胞特异性死亡,而不会波及肿瘤周围的正常组织细胞,又被通俗地称为“生物导弹”。
如今,分子靶向治疗已经不再是一个新名词,它主要包括抗体药物和小分子激酶抑制剂。不同于传统细胞毒性化疗,分子靶向治疗以肿瘤细胞的特性改变为作用靶点,在发挥更强的抗肿瘤活性的同时,减少对正常细胞的毒副作用。
随着靶向治疗的应用愈加普遍,一些在临床上较为显着的毒副作用、姑息治疗(对于手术后复发、转移或就诊时不能切除的肿瘤病人为使肿瘤缩小、稳定,以争取长期维持的化疗)的判定以及临终关怀管理问题纷至沓来。
由于患者和临床医生都乐于接受能够改善患者生活质量的新型癌症预后疗法,临床医生不仅需要了解采纳何种靶向治疗和及其临床意义,还需要了解这些靶向疗法的副作用、对患者生活质量的影响、治疗成本,尤其是如何在恰当的时间给予临终关怀的判定。
鉴于上述问题,Nature Reviews近期撰文为临床医生等相关专业人士提供了关于恶性疾病患者治疗的总结和指导。
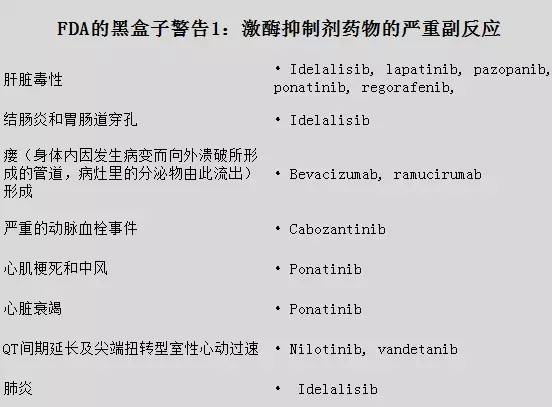
FDA批准的26款激酶抑制剂

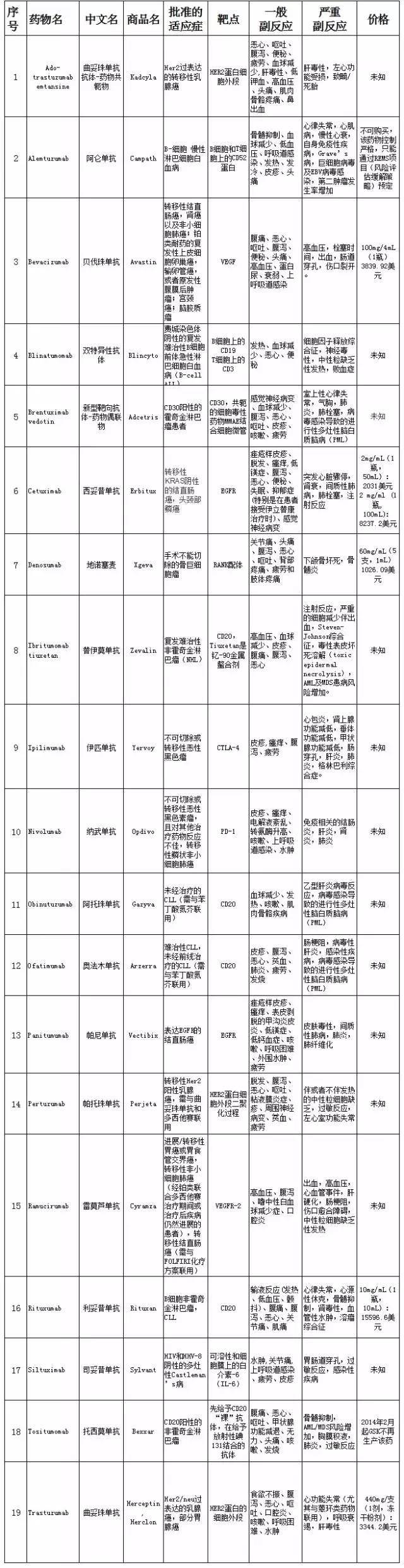
FDA批准的19款抗体药物
综上所述,在FDA批准的26款激酶抑制剂药物中,其严重不良反应可分为肝脏毒性、结肠炎和胃肠道穿孔、瘘(身体内因发生病变而向外溃破所形成的管道,病灶里的分泌物由此流出)形成、严重的动脉血栓事件、心肌梗死和中风、心脏衰竭、QT间期延长及尖端扭转型室性心动过速、肺炎,具体对应的药物见下表。
在FDA批准的19款抗体药物中,其严重不良反应可分为血球减少和输液反应、感染、胃肠道穿孔、伤口裂开/治疗问题、增加出血的风险、神经系统毒性、由于病毒感染或导致进行性多灶性白质脑病、心脏衰竭、心跳呼吸骤停和/或突然死亡、肝毒性、严重的T细胞活化、皮肤毒性、严重的过敏反应、细胞因子释放综合征、胚胎/胎儿死亡和出生缺陷,具体对应的药物见下表。

激酶抑制剂和抗体药物疗法的出现为恶性疾病的治疗提供一个重要革命。虽然一些患者在疾病早期使用上述药物具有显着的益处,有些患者甚至优于常规化疗,如使用erlotinib(埃罗替尼)及crizotinib(克唑替尼)的患者。即使是设计出设计专门针对恶性肿瘤细胞且与正常细胞具有相似的分子靶标,也不排除会有一些潜在的副作用。
尽管科学家都希望将的药物毒性降低到最低,这些新药的使用规范和不良意识还需要依赖于临床医生的用药意识和风险意识,并始终把患者的利益放在第一位,尤其是当患者在生命的最后阶段,如何恰当地给患者使用激酶抑制剂等靶向药物。
Nature Reviews客观地对FDA批准的45款靶向药物疗法进行评价,而不是一味地像其他媒体一样吹捧其治疗效果,这对于患者和医生是非常必要的。只有正确理解并妥善解决任何药物可能产生的不良效果、相关毒性,才能让患者免于接受昂贵而或无意义的治疗,也是间接地保护医疗保健系统的平衡。(生物谷Bioon.com)
相关会议推荐
2017”肿瘤免疫+”研讨会
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#副反应#
30
#FDA批准#
0
#肿瘤靶向#
45
#注意事项#
31
#Nat#
31
继续学习
73
非常好
68
#适应症#
25