Stroke:哪种降压药,对减缓小血管疾病进展最有效?
2022-05-10 Freeman MedSci原创
血管紧张素转换酶抑制剂与较少的WMH进展最一致相关,与血压控制和年龄无关。
慢性动脉高血压是脑小血管疾病(CSVD)进展的一个公认的危险因素,即放射学发现的白质高信号(WMH)。
图1 论文封面图
目前,还不清楚这种影响是完全来自于血压控制,还是次要来自于降压药物的多类特异性影响,例如钙通道阻滞剂(CCB)可以减少动脉血压的变异性。
核心假设:CCB会因减轻血压变化而减缓进展。
对未受控制的动脉高血压的治疗可降低脑小血管疾病(CSVD)进展的风险,尽管目前还不清楚这种降低是由于血压控制还是由于特定类别的多效作用,如用钙通道阻滞剂改善搏动动脉压变异性。本研究的目的是调查抗高血压药物种类的影响,特别是钙通道阻滞剂对白质增生(WMH)的影响,白质增生是CSVD的一个影像学标志,在高血压得到良好控制的队列中。
藉此,布朗大学的Eric D. Goldstein等人,完成了SPRINT-MIND试验(收缩压试验记忆和认知减少高血压)的观察性队列分析,这是一项大型随机对照试验,参与者完成了基线和4年随访的脑磁共振图像,并有体积WMH数据。
在磁共振图像之间的随访中记录了抗高血压药物治疗数据。然后得出参与者服用11类降压药中每一类的随访时间的百分比。CSVD的进展被计算为2次扫描之间WMH体积的差异,并且为了解决偏斜问题,将其分为与其余分布的最高三分位数。
在448人中,除了年龄(70.1±7.9岁对65.7±7.3岁;P<0.001)和收缩压(128.3±11.0对126.2±9.4mmHg;P=0.039)外,各WMH进展亚组的血管风险情况相似。
最高三分位数队列中的72人(48.3%)和其余队列中的177人(59.2%)都在强化血压组。处于进展最高三分位数的人的平均WMH进展为(4.7±4.3)mL,而后者为(0.13±1.0)mL(P<0.001)。
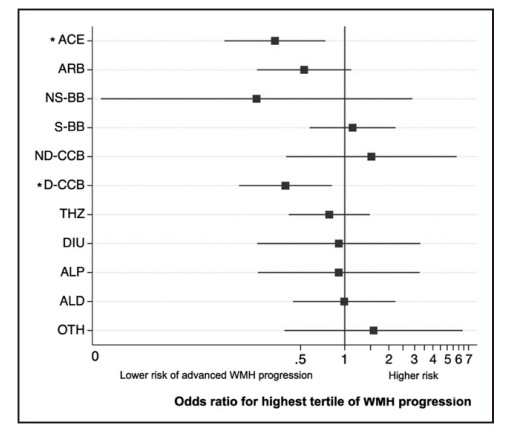
图1 不同类型降压药对WMH进展影响
使用血管紧张素转换酶抑制剂(几率比,0.36 [95% CI,0.16-0.79];P=0.011)和二氢吡啶类钙通道阻滞剂(几率比,0.39 [95% CI,0.19-0.80];P=0.011)与较少的WMH进展有关,尽管当WMH被视为一个连续变量时,二氢吡啶类钙通道阻滞剂失去意义。
该研究的重要意义在于发现了:在SPRINT-MIND试验的参与者中,血管紧张素转换酶抑制剂与较少的WMH进展最一致相关,与血压控制和年龄无关。
原文出处:
Goldstein ED, Wolcott Z, Garg G, et al. Effect of Antihypertensives by Class on Cerebral Small Vessel Disease: A Post Hoc Analysis of SPRINT-MIND. _Stroke_. Published online May 4, 2022:10.1161/STROKEAHA.121.037997. doi:[10.1161/STROKEAHA.121.037997](https://doi.org/10.1161/STROKEAHA.121.037997)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#小血管疾病#
32
#疾病进展#
49
很好,临床课题,很有意义!
46
学习了,谢谢分享
39
#降压#
39
#血管疾病#
34