大样本结果显示结直肠癌cfDNA与组织样本一致性近乎100%
2017-12-03 生信者言 生信者言
2017年12月1日,来自麻省总医院癌症中心与MD安德森癌症中心的研究团队在著名学术杂志Cancer Discovery在线发表题为“Genomic landscape of cell-free DNA in patients with colorectal cancer”的研究论文。 该研究报道了1397例结直肠癌患者cfDNA的NGS研究结果,总体而言,在cfDNA中检测到的基因
2017年12月1日,来自麻省总医院癌症中心与MD安德森癌症中心的研究团队在著名学术杂志Cancer Discovery在线发表题为“Genomic landscape of cell-free DNA in patients with colorectal cancer”的研究论文。
该研究报道了1397例结直肠癌患者cfDNA的NGS研究结果,总体而言,在cfDNA中检测到的基因变异频率与在三个基于组织样本的研究中得到的结果近乎完全一致。另外,作者还分析鉴定了EGFR基因中一组新的胞外域(ECD,extracellular domain )突变,这些突变通过阻断anti-EGFR抗体的结合来介导相关靶向药物的耐受。具有EGFR ECD突变的患者显示明显的肿瘤异质性,其中91%具有多个不同的耐药突变。
cfDNA与肿瘤组织突变谱比较
作者分析了来自1,772个CRC患者的连续血液样本,这些患者在2014年6月1日至2016年5月18日之间接受了Guardant360的靶向NGS检测。其中,有1500例(85%)患者的cfDNA中至少有一个可检测到的基因突变;请注意,这1500例中,有103个样品属于同一患者的连续血液样本;因此,最终剩余1,397名具有基因突变的患者进行后续分析。
注:Guardant360为Guardant Health推出的一项肿瘤分子检测产品,本研究期间共涉及三个panel:54 gene panel、68 gene panel、70 gene panel。

将在cfDNA中检测到的非同义单核苷酸突变(SNV)的频率分别与TCGA数据库(n=228)、NHS/HPFS(n=619)、GENIE(n=1149)这三个基于组织检测结果的公开数据库进行比较。
注:NHS/HPFS全称为: Nurses Health Study/Health Professionals Follow-Up Study
GENIE全称为: Genomics Evidence Neoplasia Information Exchange
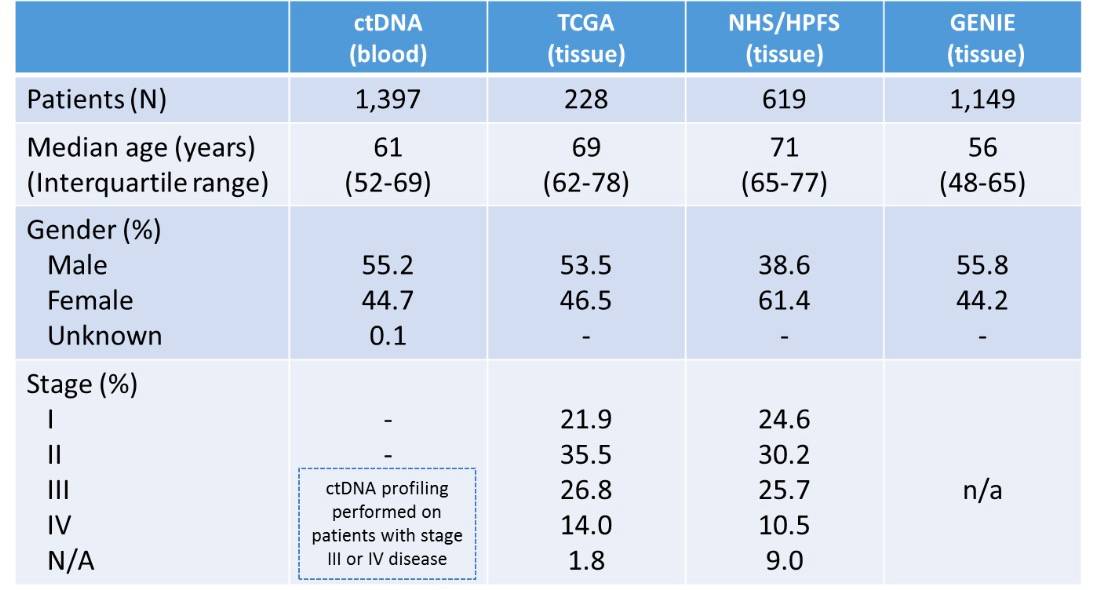
患者统计资料(第1列为该研究,以cfDNA样本进行测序;第3/4/5列是对组织样本进行测序的三个研究队列,用作对照)
为了保持比较过程的统一,研究者将参与比较的所有队列调整为只包括cfDNA检测所涵盖的那些SNV。结果发现,cfDNA检测结果与组织样本的研究之间突变发生率基本一致。
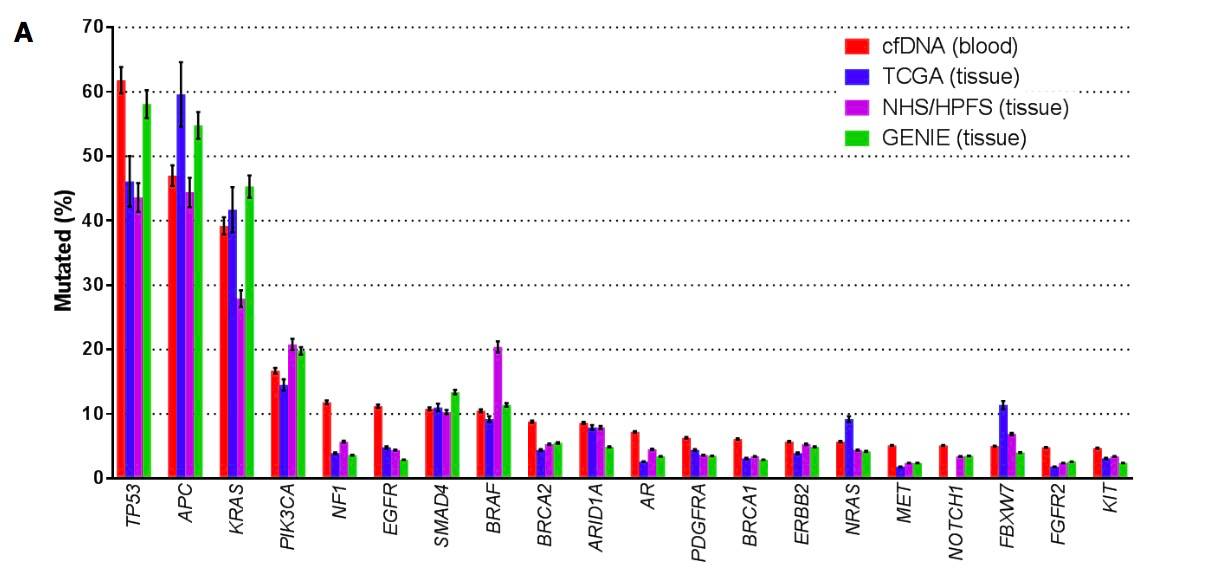
Fig:Comparison of mutation frequencies in cfDNA and tissue cohorts
对于这些非常小的差异,作者的解释是:这可能是由于统计差异造成的,或者是因为这三个基于组织样本队列的人口统计学差异。例如,NHS / HPFS队列中BRAF突变率增加可能是由于该队列中女性比例较大。
注:BRAF突变在女性CRC患者中更常见
总体而言,cfDNA检测得到的结果与三种基于组织的数据库之间的突变率具有惊人的相似性!
cfDNA中20个最常发生突变的基因,其突变率与肿瘤组织样本中的突变频率有很高的相关性(R2= 0.95; p<0.0001)。尽管如此,cfDNA和组织样本之间还是有一些较为显著的差异。例如,EGFR突变在cfDNA中的突变频率(11.2%)比在组织样本中的突变频率(4.8%for TCGA;4.4%for NHS / HPFS;2.9% for GENIE)更高。
这种较为显著的差异可能反映了cfDNA和基于组织的队列之间真正的生物学差异,因为接受cfDNA检测的患者更有可能存在转移病灶并且之前已接受过治疗。
另外,如上图C所示:
在16名患者的cfDNA中检测到JAK2 基因的V617F突变,但是在组织样本中完全没检测到。这种差异最可能的解释是在cfDNA中检测到的JAK2 V617F突变实际上并不存在于患者的肿瘤中,而是存在于功能不明的造血克隆(hematopoietic clone )中,这种情况在0.2%的人群中有观察到。
事实上,JAK2 V617F突变是在造血克隆中观察到的最常见突变之一,并且这些突变会随着年龄增长而增加。
与此假设一致的现象是,我们发现上图D中,cfDNA中检测到JAK2 V617F突变的患者的中位年龄为73岁,而没有这种突变的患者中位年龄为60。
这个例子正好说明:基于血液的基因分析有一个很大的限制,即无法判断cfDNA中检测到的突变真的就是从患者的肿瘤中获得的。
尽管如此,这些数据总体上表明,基于cfDNA和基于组织的基因检测结果之间的相似性非常高,并且总体上支持大规模进行cfDNA基因组分析的潜在价值和有效性
比较克隆突变与亚克隆突变
先对“克隆”与“亚克隆”进行一个定义。
如果突变等位基因频率(mutant allele frequency,MAF)小于样品中最高MAF的25%,则将突变定义为“亚克隆”;如果高于该阈值,则将其定义为“克隆”。

Fig:Proportion of clonal vs. subclonal mutations in commonly mutated genes in cfDNA
在51%的患者中,至少发现一个亚克隆突变(数量范围是1~54个);cfDNA中突变率最高的20个基因中,有6个基因是克隆突变,包括KRAS,FBXW7,APC,SMAD4,BRAF和TP53。这些基因都已知在CRC的发病中参与早期、关键事件。
此外,如下图所示,克隆SNV被预测可能会激活或失活那些肿瘤发生过程的driver mutations,而亚克隆SNV更可能是不起作用的“passenger” mutations 或者意义未明。

Fig:Impact of variant functional significance on clonality of the alteration.
我们假设另一类亚克隆突变可能代表在先前治疗期间出现的“non- truncal获得性耐药突变”,有趣的是,EGFR基因上的亚克隆突变百分比最高。
如下图右边所示,当两个主要的克隆性突变(KRAS和APC)的MAF在个体肿瘤中进行比较时,我们观察到很好的线性关系,表明这些突变在CRC中常常作为克隆事件共存,尽管这个过程中也有一些亚克隆性的突变,如某些KRAS和APC突变。
然而,如下图左边所示,当比较EGFR基因和APC基因的SNV的MAF时,未观察到线性关系,即大多数EGFR突变发生在亚克隆频率,这表明在cfDNA中检测到的EGFR基因突变不可能在CRC发展中成为克隆事件,而是可能是作为肿瘤进展或转移时的特定亚克隆,或也许是为了回应抗癌疗法的选择性压力。与这种假设相一致,EGFR基因亚克隆突变的许多患者,其EGFR基因的胞外结构域(ECD)中存在特定的突变。
类似地,许多KRAS亚克隆突变也发生在这些具有EGFR ECD突变的患者中。
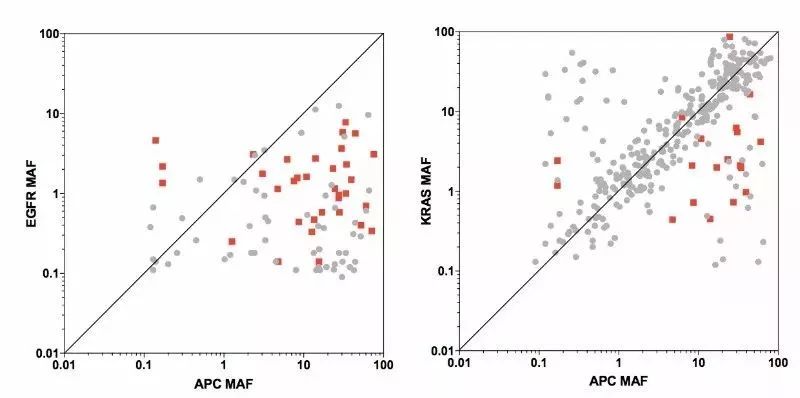
KRAS和NRAS(RAS)突变是另一个在anti-EGFR抗体治疗时可能出现的一种常见的获得性耐药机制,并且先前的研究已经显示在anti-EGFR治疗时,同一患者会同时出现亚克隆性RAS突变和EGFR ECD突变。
上文提到,cfDNA比组织样本中EGFR的突变频率更高,这也反映了亚克隆抗性突变的出现,特别是在EGFR抗体治疗获得性耐药时。
cfDNA中EGFR基因的胞外域突变
重点分析EGFR突变患者,如下图所示,157例EGFR突变患者中有85例在胞外结构域发生突变。
为了鉴定哪些突变与功能的相关性最大,作者准备重点研究在该群组中重复出现的EGFR ECD突变(在一个以上的患者中观察到),总共有58位患者符合要求。其中,42位患者的EGFR ECD突变发生在EGFR基因的结构域III中,这个区域是与西妥昔单抗和帕尼单抗的结合表位。
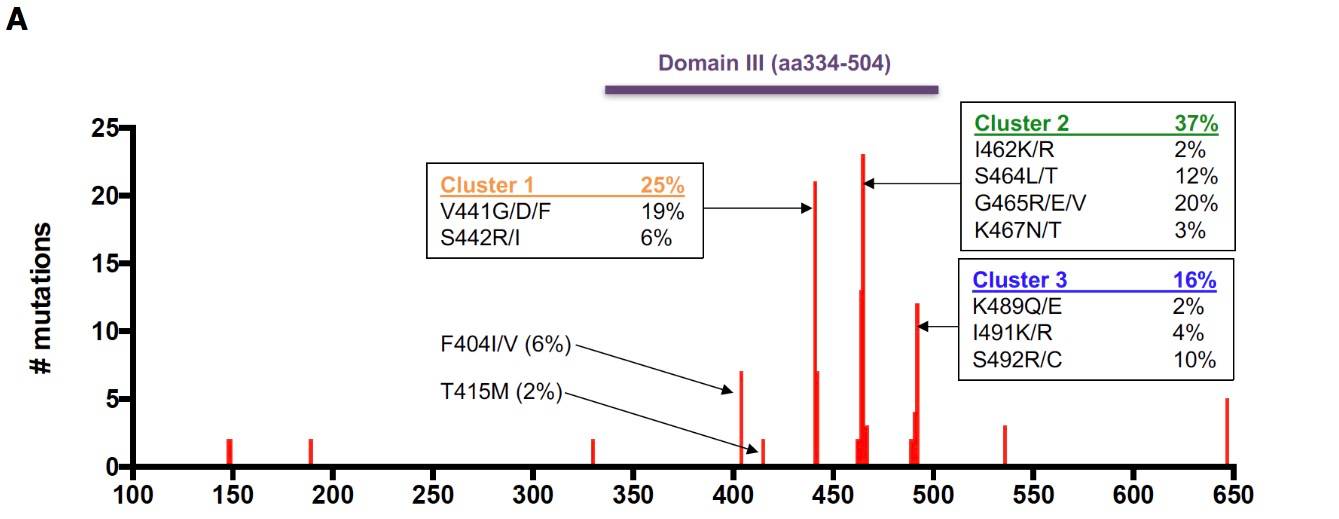
Fig:EGFR ECD mutations occurring more than once in cfDNA cohort
在这42位患者中,有24位(57%)在采血前进行过anti-EGFR抗体治疗,这支持了这些突变在耐药方面的作用。其余18名患者的治疗史未知。
对这42位患者的EGFR ECD突变进行分析,揭示了结构域III中11个氨基酸的23个不同的突变。
在小部分患者中观察到F404和T415突变,以前没有被报道过anti-EGFR抗体耐药性。然而,先前未涉及anti-EGFR抗体耐药的V441和S442的形成了新簇(Cluster 1),占所有EGFR ECD突变的25%。这些新颖且重复出现的突变中的大多数,会影响V441,V441D和V441G。

为了验证这种新的获得性耐药机制,作者进行了分子建模来预测这些突变对西妥昔单抗与EGFR结合的影响。最终发现,V441D和V441G EGFR突变体与野生型EGFR相比,西妥昔单抗和帕尼单抗的结合力显著降低。
证明EGFR ECD突变是一种获得性耐药的新机制。
anti-EGFR抗体治疗耐药的异质性
为了进一步研究肿瘤异质性对获得性耐药后的治疗策略有何影响,研究者继续对42例EGFR ECD突变患者的cfDNA图谱进行深入分析。
除了EGFR ECD突变之外,之前已经知道的anti-EGFR抗体获得性耐药机制,包括KRAS,NRAS,BRAF,MAP2K1,ERBB2,MET和KIT基因的突变。
我们观察到,91%具有EGFR ECD突变的患者中,还会检测到至少另一个耐药突变,平均一般有5个突变。而在单个患者中,可检测到多达13个同时发生的耐药突变,表明存在着显著的异质性。
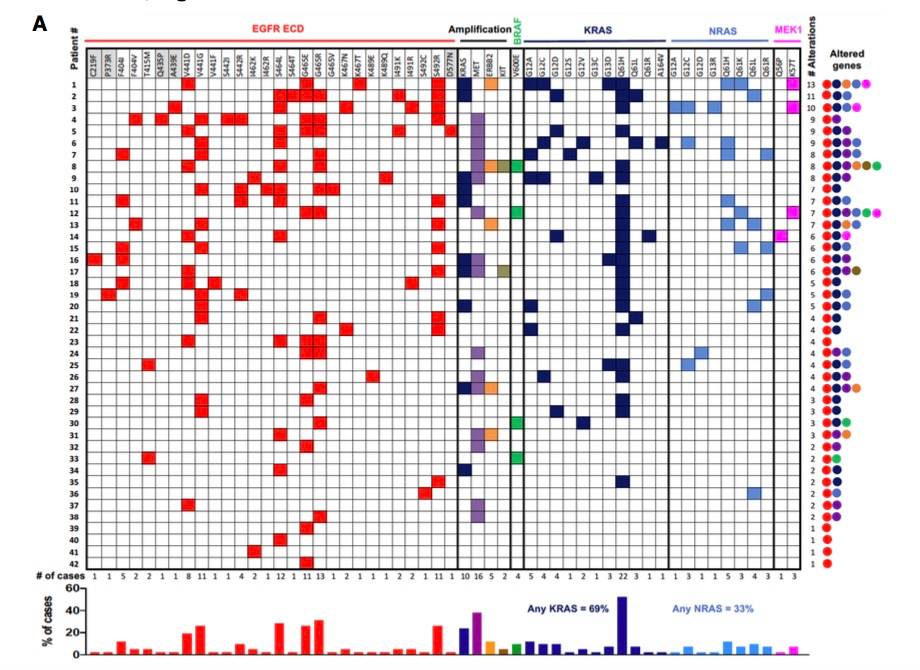
Fig:Heterogeneity of anti-EGFR resistance alterations in patients with EGFR ECD mutations
KRAS突变(包括扩增)是观察到的最常见的耐药突变,存在于69%的患者中。MET扩增,NRAS突变和KRAS扩增也很常见,分别占38%,33%和24%; BRAF和MAP2K1突变均占9.5%。
在个体患者的cfDNA中存在多个耐药突变被认为代表在治疗期间出现的多个耐药亚克隆的存在,其可能存在于不同转移灶中。
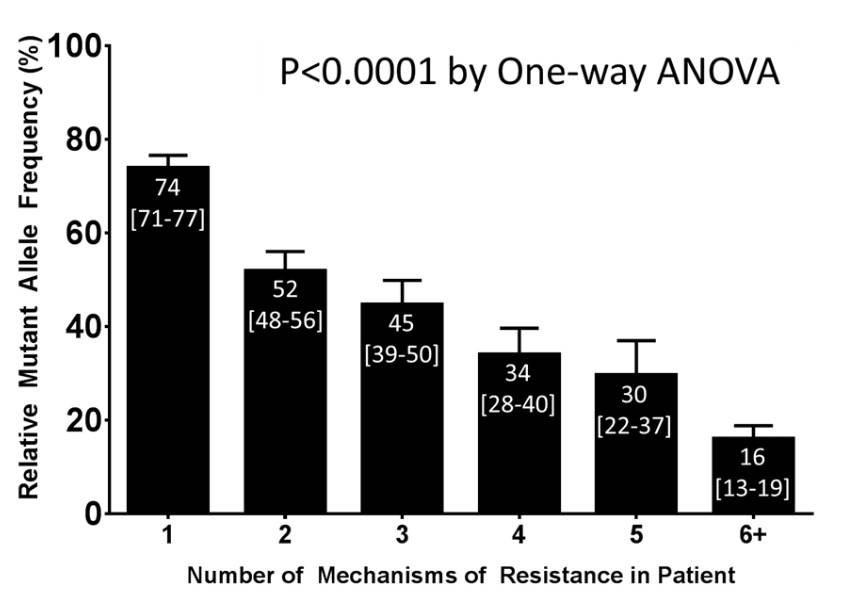
Fig:Relationship between number of concurrent resistant mechanisms and relative mutant allele frequency of resistance alterations.
与此模型相一致的是,如上图所示,存在多个耐药突变的患者与只有一个耐药突变的患者相比,他的这些耐药突变都是亚克隆。简单理解就是,突变数目多的,突变频率相应的低。
如下图展示的三个患者,分析还揭示了在获得性耐药时会发生显著的异质性。每个患者的突变情况都不同。
例如,一名患者(下图,pt#1)具有13种不同的抗性突变,包括4种EGFR ECD突变,4种KRAS突变,KRAS扩增,2种NRAS突变,ERBB2扩增和影响MEK1的下游突变(由MAP2K1编码)。
为了克服获得性耐药,已经开发了anti-EGFR抗体混合物,如Sym004和MM-151,其能够结合EGFR上的多个表位,并且可以克服单个EGFR ECD的耐药突变效应。然而,这些药物也许不能克服非ECD的耐药突变,这种耐药突变通过在RAS-RAF-MEK-ERK途径中的其他点处的活化而绕过对EGFR信号传导的需求。
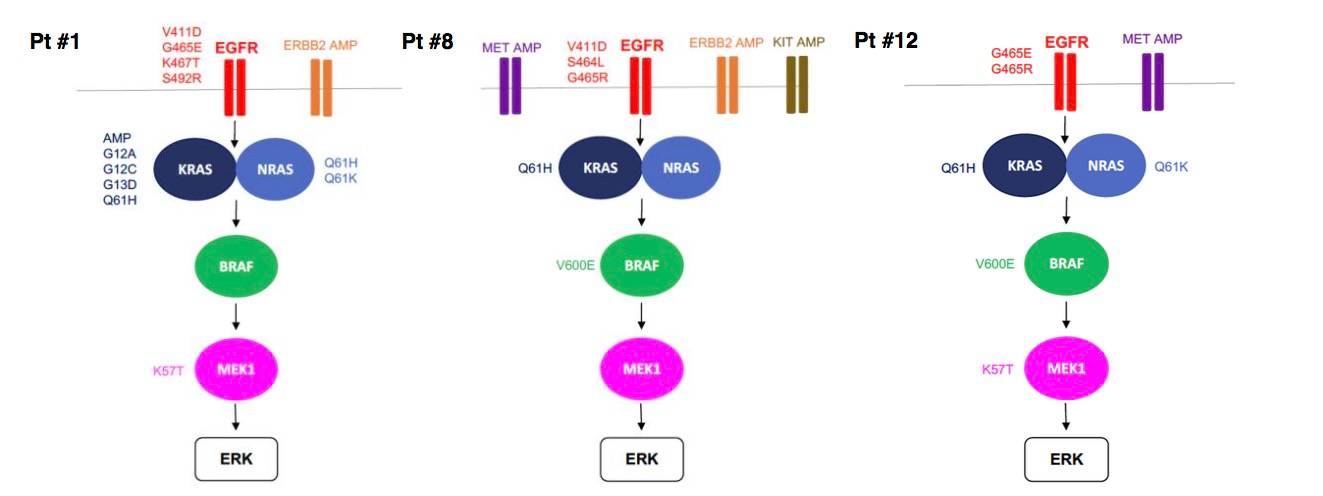
Fig:Case examples of patients with multiple EGFR pathway alterations.
总的来说,这项研究支持大规模cfDNA分析的潜在应用,以了解癌症患者的基因组图谱,并提供新的视角以了解肿瘤异质性和耐药问题。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#样本#
45
#cfDNA#
33
#一致性#
38
#结直肠#
61
学习一下谢谢分享
66
学习了受益匪浅
57
谢谢分享学习了
59