Cardiovasc Diabetol:住院与非住院肥胖受试者的Galectin-4水平
2022-09-04 MedSci原创 MedSci原创
人们一直在猜测某些肥胖个体如何降低患心血管疾病和2型糖尿病(DM2)的风险,从而显示出肥胖作为一种风险因素的异质性。

背景:肥胖(体重指数,身体质量指数≥30 kg/m2)会导致健康并发症,并缩短预期寿命约20年。这主要是因为患许多非传染性疾病的风险显著增加,如二型糖尿病(T2DM)、心血管疾病和某些类型的癌症。更麻烦的是,自20世纪70年代以来,全球肥胖患病率一直在稳步上升,尤其是在青少年和儿童中,今天已达到疫情水平。尽管肥胖与心血管疾病风险增加之间的联系本身并不存在争议,但长期以来,人们一直在猜测某些肥胖个体如何降低患心血管疾病和2型糖尿病(DM2)的风险,从而显示出肥胖作为一种风险因素的异质性。
此外,尽管从流行病学的角度来看,肥胖的心脏代谢并发症已经得到了很好的证实,但其潜在的病理生理学机制尚未完全了解,特别是考虑到肥胖的异质性时。最近,在将多组学用于探索特定细胞类型的改变和识别促进疾病发展的信号事件的改变方面,已经取得了相当大的技术进步。为了更好地了解肥胖症疾病进展背后的机制,我们应用邻近延伸分析(PEA)技术来测量与炎症和CVD相关的92种蛋白质(生物标记物)。这代表了一种探索多种蛋白质和生物系统之间的联系的有吸引力的方法,这反过来可能呈现出可能的诊断、预后和治疗意义。
目的:这项以人群为基础的横断面研究的目的是探索CVD生物标志物和不健康肥胖表型之间可能的新关联,即使用由92种与心血管疾病相关的蛋白质组成的多元蛋白质组平台,对有躯体疾病住院史直至中年晚期的肥胖受试者进行研究。
方法:分析了517例(平均年龄67±6岁;33.7%的女性)来自马尔默预防项目队列的肥胖(身体质量指数≥30 kg/m2)个体,使用Olink CVD III小组的邻近延伸阵列技术。在研究基线前至少有一次因躯体疾病住院记录的个体被定义为HO表型。蛋白质和HO (n = 407)与非住院肥胖受试者(NHO,n = 110)之间的关系,使用多变量二元逻辑回归分析,调整传统的危险因素。
结果:在92个分析过的生物标记物和HO之间的未调整关联中,两种蛋白水平的增加在假发现率< 0.05时是显著的:Galectin-4 (Gal-4)和胰岛素样生长因子结合蛋白1 (IGFBP1)。当这两种蛋白被包括在校正了年龄和性别的逻辑回归分析中时,Gal-4仍然是显著的。在多变量逻辑回归分析中,Gal-4与HO表型独立相关(OR 1.72CI95 % 1.16–2.54)。事后分析显示,这种关联只存在于糖尿病亚人群中(OR 2.26CI95 % 1.25–4.07)。然而,进行了相互作用分析,显示Gal-4和流行性糖尿病之间没有显著的相互作用(p = 0.16)。
表1显示Galectin-4水平和HO概率之间关系的逻辑回归模型
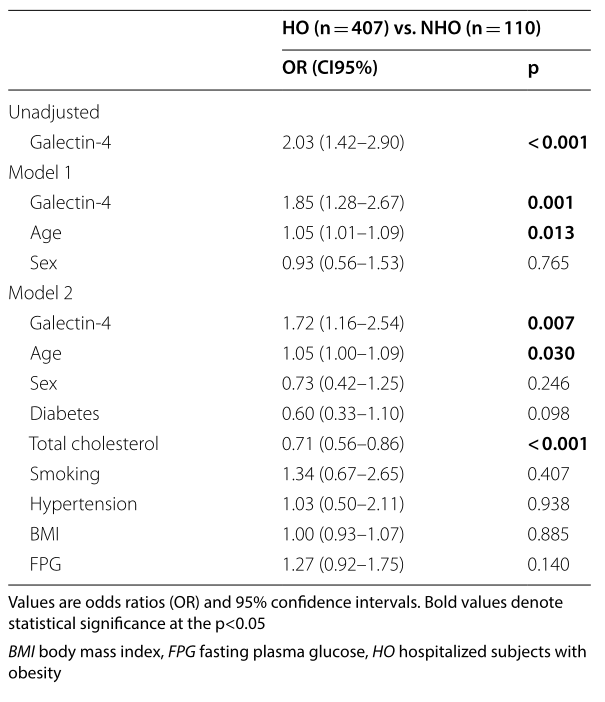
表2比较患有或不患有流行性糖尿病的肥胖受试者中Gal-4水平的事后分析
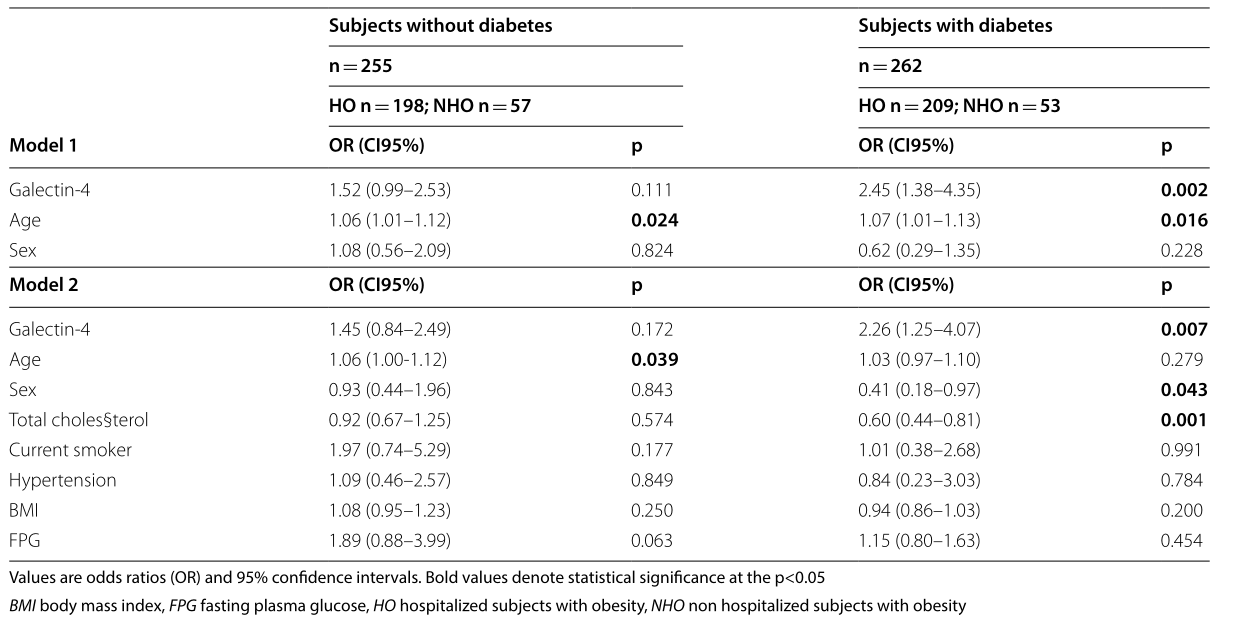
结论:在中老年肥胖个体中,Gal-4水平升高与HO的高概率相关。这种相关性仅在糖尿病患者中有意义,进一步暗示了Gal-4在糖尿病及其并发症中的作用。
原文出处:
Korduner J, Holm H, Jujic A, et al.Galectin-4 levels in hospitalized versus non-hospitalized subjects with obesity: the Malmö Preventive Project.Cardiovasc Diabetol 2022 Jul 02;21(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#BET#
50
#DIA#
39
#ASC#
43
#受试者#
39