Circulation: 镰刀型细胞病患者动脉硬化损伤与慢性血管并发症有关
2016-09-30 xing.T MedSci原创
由此可见,颈-股动脉脉搏波速度和增强指数在镰状细胞病患者内发生很大的改变,这些变化不仅与较低血压和较高心率存在独立相关性,而且也与血红蛋白表型存在相关性。此外,颈-股动脉脉搏波速度和增强指数与几种镰状细胞病临床并发症密切相关,提示它们在患者后续的随访中有重要的评估预后的价值。
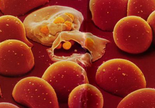
作为血液系统遗传性疾病的镰刀状细胞疾病可导致多器官受累的慢性血管病变。最近,心血管领域权威杂志《Circulation》上发表了旨在探究镰刀状细胞疾病动脉硬化与慢性血管相关并发症的关系的研究。
研究者纳入了3627例镰刀状细胞病患者和943例对照者,研究者发现相比于对照组(9.1±2.4 m/s,p<0.0001),镰刀状细胞病患者的平均颈-股动脉脉搏波速度较低(7.5±2m/s),心率校正后,增强指数在镰刀状细胞病患者中随年龄增长上升地更迅速,并且比对照组患者水平更高。颈-股动脉脉搏波速度和增强指数与年龄、性别、身高、心率、平均动脉压、血红蛋白水平、地域和血红蛋白表型独立相关。对这些关联进行调整后,颈-股动脉脉搏波速度和增强指数与肾小球滤过率、股骨头坏死有关。增强指数也与脑卒中、肺动脉高压和异常勃起有关,而颈-股动脉脉搏波速度与微量白蛋白尿相关。
由此可见,颈-股动脉脉搏波速度和增强指数在镰状细胞病患者内发生很大的改变,这些变化不仅与较低血压和较高心率存在独立相关性,而且也与血红蛋白表型存在相关性。此外,颈-股动脉脉搏波速度和增强指数与几种镰刀状细胞病临床并发症密切相关,提示它们在患者后续的随访中有重要的评估预后的价值。
原始出处:
Brigitte Ranque, et al. Arterial Stiffness Impairment in Sickle Cell Disease Associated With Chronic Vascular Complications. Circulation. 2016.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#并发#
24
好文章,受益
54
收藏
55
继续关注
58
继续学习
57
#损伤#
33
#血管并发症#
20
继续关注
59
继续学习
21
谢谢分享,阅读了。
27