JAHA:低盐高钾饮食对动脉僵度和左心室功能的影响
2021-12-08 MedSci原创 MedSci原创
该研究的结果表明,限制钠盐可能不会改变动脉和左室硬度。但有必要进行纵向研究以阐明饮食对动脉和左心室功能的影响。
限钠饮食是可改善血压、动脉僵硬度和左心室舒张功能潜在的非药物策略。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员调查了与年龄相关的左心室结构和功能差异,以及评估保持传统生活方式(包括低盐和高钾饮食)的土著巴布亚人左心室功能与中心血流动力学之间的关系。

研究人员通过超声心动图和多普勒成像测量了受试者的左心室大小、二尖瓣血流量和二尖瓣环组织速度。研究人员使用自动血压计(欧姆龙)测量了血压和臂踝脉搏波速度,并通过示波法(Mobil-O-Graph,使用欧洲校准)估计了受试者中心血压和波反射参数。
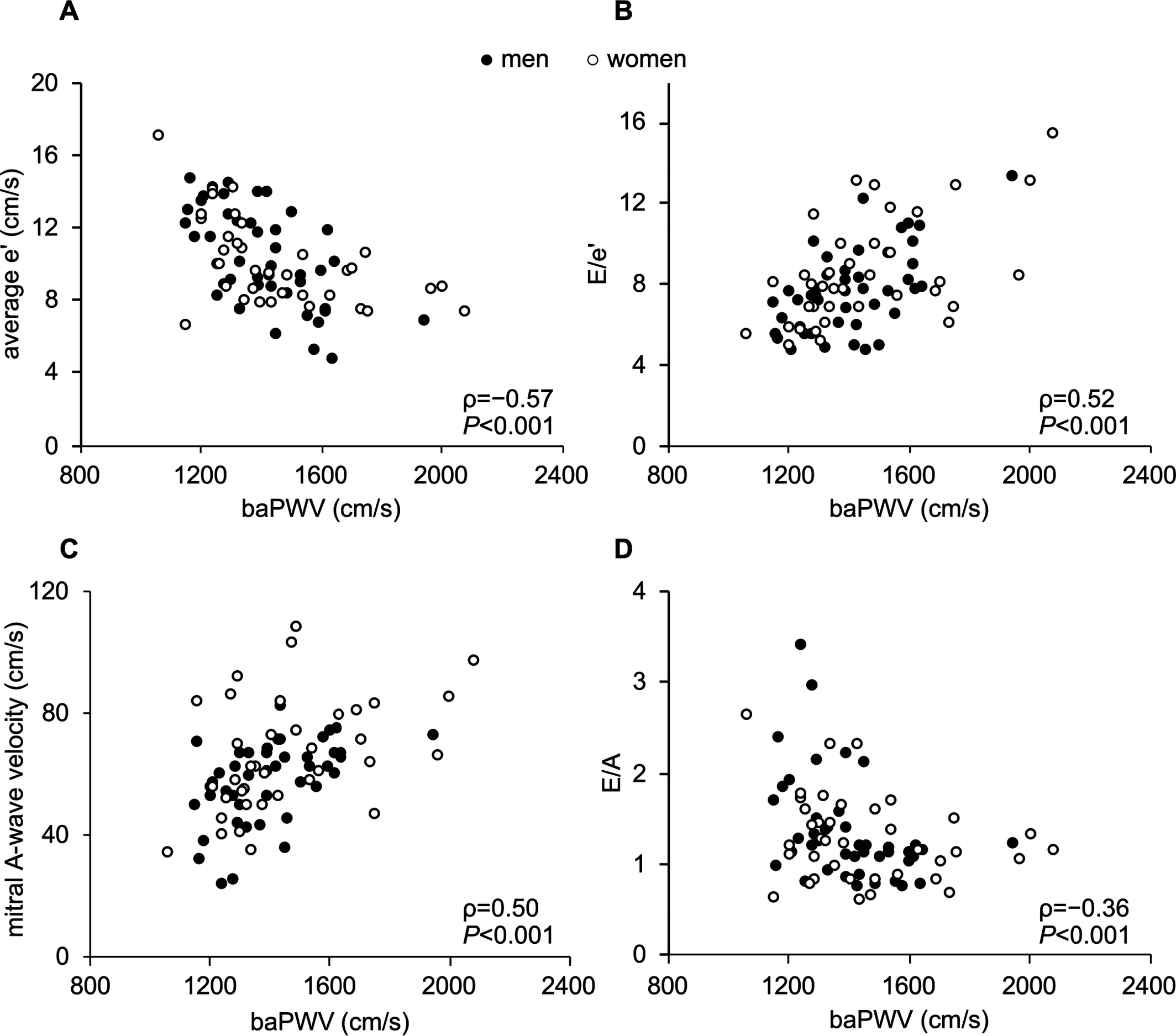
该研究共纳入了82名巴布亚本地人(中位年龄为42岁;38名女性;未接受血压治疗)。年龄相关的臂收缩压差异不大但显著,臂踝脉搏波速度随年龄显著增加;然而,左心室质量指数保持不变。左心室射血分数和整体纵向应变正常;二尖瓣A波速度和平均E/e´增加;e´和E/A随年龄增长而下降。臂踝脉搏波速度和尿Na/K与E/e´呈正相关且独立相关。年龄和心率与E/A呈负相关。总之,左室收缩功能正常;然而,巴布亚人的左心室舒张功能随着年龄的增长而下降。此外,与年龄相关的动脉硬化,而不是波反射,与左心室舒张功能呈负相关。
由此可见,该研究的结果表明,限制钠盐可能不会改变动脉和左室硬度。但有必要进行纵向研究以阐明饮食对动脉和左心室功能的影响。
原始出处:
Akio Ishida,et al.Effects of a Low‐Salt and High‐Potassium Diet on Arterial Stiffness and Left Ventricular Function in Indigenous Papuans.JAHA.2021.https://www.ahajournals.org/doi/full/10.1161/JAHA.121.021789
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#AHA#
28
#左心室#
44
#高钾#
32
认真学习了。
44