Heart:术前肾功能不全与TAVI患者转归差相关
2015-02-05 高晓方 译 医学论坛网
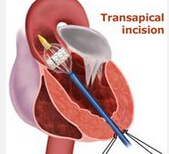
英国一项研究表明,在接受经导管主动脉瓣置入术(TAVI)的患者中,术前肾功能不全与包括死亡在内的转归恶化具有相关性。论文1月12日在线发表于《心脏》(Heart)。 此项研究利用TAVI登记系统前瞻性采集了3980例患者的相关数据和临床转归资料,并评估了肾功能不全与TAVI后患者转归的相关性。 结果显示,205例(5.5%)患者在住院期间死亡。即便对危险因素进行校正之后,中、重度慢
英国一项研究表明,在接受经导管主动脉瓣置入术(TAVI)的患者中,术前肾功能不全与包括死亡在内的转归恶化具有相关性。论文1月12日在线发表于《心脏》(Heart)。
此项研究利用TAVI登记系统前瞻性采集了3980例患者的相关数据和临床转归资料,并评估了肾功能不全与TAVI后患者转归的相关性。
结果显示,205例(5.5%)患者在住院期间死亡。即便对危险因素进行校正之后,中、重度慢性肾病(CKD)与死亡率升高仍具有显著相关性(P=0.04)。eGFR每降低10 mL/min/1.73 m2,院内死亡率升高8.2%。
在随访期间死亡的1119例患者中,即使是校正危险因素后,中、重度CKD (eGFR <45 mL/min/1.73 m2)与死亡率升高显著相关;eGFR每降低10 mL/min/1.73 m2,累积死亡率升高4.4%。术前生功能和术后透析需要可预测临床转归。
原始出处:
Ferro CJ1, Chue CD1, de Belder MA2, Moat N3, Wendler O4, Trivedi U5, Ludman P1, Townend JN1; On behalf of the UK TAVI Steering group and the National Institute for Cardiovascular Outcomes Research.Impact of renal function on survival after transcatheter aortic valve implantation (TAVI): an analysis of the UK TAVI registry.Heart. 2015 Jan 12. pii: heartjnl-2014-307041. doi: 10.1136/heartjnl-2014-307041. [Epub ahead of print]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#肾功能#
24
已阅
114
已阅
127
好好好
114
#肾功能不全#
27
#ART#
30
#HEART#
23