Cancer Cell:区分肾癌亚型 有前景的新药靶点
2012-01-06 MedSci原创 MedSci原创
Van Andel研究所的科学家近期的研究为更完整地了解肾癌不同亚型奠定了基础,这可能为更好地治疗方法铺平了道路。 由Kyle Furge博士和Aikseng Ooi博士发表于Cancer Cell上的一项研究中,研究者对2型乳头状肾细胞癌(PRCC2)提供了一个更为完整的理解,这为开发有效的治疗策略奠定了基础(注:PRCC2是一种恶性肾癌,目前没有有效的疗法)。 尽管具有明显的形态学、遗传学
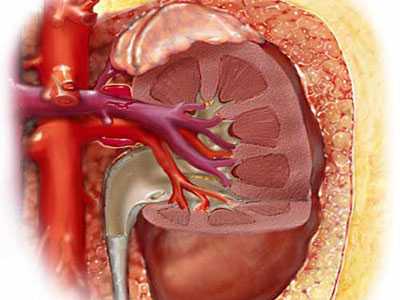
Van Andel研究所的科学家近期的研究为更完整地了解肾癌不同亚型奠定了基础,这可能为更好地治疗方法铺平了道路。
由Kyle Furge博士和Aikseng Ooi博士发表于Cancer Cell上的一项研究中,研究者对2型乳头状肾细胞癌(PRCC2)提供了一个更为完整的理解,这为开发有效的治疗策略奠定了基础(注:PRCC2是一种恶性肾癌,目前没有有效的疗法)。
尽管具有明显的形态学、遗传学和临床上的差异,遗传型PRCC2被认为与另一种肾癌--肾透明细胞癌(CCRCC)有相似的基于基因突变所致的信号通路失调。CCRCC是肾癌的一个亚型,约占肾癌的75%,与PRCC2不同,它对靶向血管内皮生长因子(VEGF,细胞中的一种信号蛋白,能够刺激血管的形成)的药物积极响应。
该研究是同其他国际学者共同协作完成,包括新加坡国立癌症中心、EPFE-INSERM U753遗传肿瘤所、巴黎Sud医学院、Gustave Roussy癌症研究所、密歇根州立大学、西北纪念医院、克利夫兰诊所、新加坡中央医院、Wistar研究所,鉴定出KEAP1-NRF2信号通路的放松管制是区别PRCC2和CCRCC的一个因素,但与遗传型及散发型PRCC2相关。
在另一项发表于癌症研究中的研究(由Yan Ding博士和Bin Tean Teh博士与新加坡国立癌症研究中心合作进行的)中,研究人员综合了基因表达谱和RNAi筛选数据来鉴定与CCRCC发生和发展相关的基因。
近年来,一些分子靶向疗法如舒尼替尼、索拉非尼、帕唑帕尼这些靶向血管内皮生长因子的酪氨酸激酶受体已被批准用于治疗CCRCC。尽管这些疗法能显著的延长患者的总生存期,但最终几乎所有的CCRCC患者仍无法逃过病魔。
基因组富集分析表明,细胞周期相关的基因,尤其是PLK1,与疾病的侵略性相关。此外,PLK1与疾病的侵染和体外生长促使研究人员检测小分子抑制剂对CCRCC细胞系的抑制作用。他们的研究结果强调PLK1是治疗CCRCC的非常有潜力的靶标。(生物谷bioon.com)
An Antioxidant Response Phenotype Shared between Hereditary and Sporadic Type 2 Papillary Renal Cell Carcinoma
Aikseng Ooi, Jing-Chii Wong, David Petillo, Douglas Roossien, Victoria Perrier-Trudova, Douglas Whitten, Bernice Wong Hui Min, Min-Han Tan, Zhongfa Zhang, Ximing J. Yang, Ming Zhou, Betty Gardie, Vincent Molinie, Stephane Richard, Puay Hoon Tan, Bin Tean Teh, Kyle A. Furge
Summary :Fumarate hydratase (FH) mutation causes hereditary type 2 papillary renal cell carcinoma (PRCC2). The main effect of FH mutation is fumarate accumulation. The current paradigm posits that the main consequence of fumarate accumulation is HIF-α stabilization. Paradoxically, FH mutation differs from other HIF-α stabilizing mutations, such as VHL and SDH mutations, in its associated tumor types. We identified that fumarate can directly up-regulate antioxidant response element (ARE)-controlled genes. We demonstrated that aldo-keto reductase family 1 member B10 (AKR1B10) is an ARE-controlled gene and is up-regulated upon FH knockdown as well as in FH null cell lines. AKR1B10 overexpression is also a prominent feature in both hereditary and sporadic PRCC2. This phenotype better explains the similarities between hereditary and sporadic PRCC2.
Highlights :Increased expression of AKR1B10 is a prominent feature of FH null cells ? Fumarate mediates the stabilization of NRF transcription factors ? The KEAP1-NRF axis is deregulated in type 2 papillary renal cell carcinomas ? Complete gene expression profiles of FH null kidney cancers are presented.
Significance :Type 2 papillary renal cell carcinoma (PRCC2) is an aggressive disease with no effective treatment. Despite the obvious orphological, genetic, and clinical differences, hereditary PRCC2 is thought to share similar pathway deregulation with ts clear-cell counterpart (CCRCC) that arises as a result of SDH or VHL mutation. Furthermore, the robust response seen ith anti-VEGF agents in CCRCC is not reproducible in PRCC2. This represents a distinct knowledge gap in the understanding of PRCC2 biology. We identi?ed deregulation of the KEAP1-NRF2 axis as a feature that distinguishes PRCC2 rom CCRCC, but links both hereditary and sporadic PRCC2. Therefore, our finding provides a more complete understanding of PRCC2 biology and lays the foundation for the development of effective treatment strategies.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#有前景#
41
#Cell#
41
#CEL#
53
#cancer cell#
39