Journal of Oncology Practice:一项对药物监测的前瞻性研究——癌症患者联合用药的药物间相互作用
2017-06-25 MedSci MedSci原创
癌症患者经常使用草药补充剂和抗肿瘤化疗药物进行联合治疗。在这些患者中,草药-化药相互作用(HDI)和药物-药物相互作用(DDI)的风险较高。6月19日发表在《肿瘤学实践》杂志上的一项研究表明,其中一些具有临床意义。研究人员通过给病人们做一份问卷调查,启动了一种新的抗癌疗法,以记录任何非处方药物或草药补充剂与化疗药的联合使用。并通过两个不同的数据库识别潜在的DDI和HDI。如果临床药师发现有潜在的临
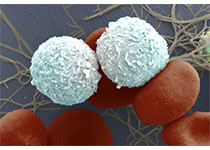
癌症患者经常使用草药补充剂和抗肿瘤化疗药物进行联合治疗。在这些患者中,草药-化药相互作用(HDI)和药物-药物相互作用(DDI)的风险较高。6月19日发表在《肿瘤学实践》杂志上的一项研究表明,其中一些具有临床意义。
研究人员通过给病人们做一份问卷调查,启动了一种新的抗癌疗法,以记录任何非处方药物或草药补充剂与化疗药的联合使用。并通过两个不同的数据库识别潜在的DDI和HDI。如果临床药师发现有潜在的临床相关的DDI,就会向开处方的肿瘤学家发出通知,他们决定是否进行药物干预。研究人员对患者的临床相关的DDIs和HDIs进行了检查。并对结果进行了回归分析,以确定与临床相关的DDIs相关的变量。
本研究共纳入149例患者,其中有26例(17.4%; 95%置信区间,11.3%至23.5%)鉴定出36种潜在临床相关的DDI,所有的这些的治疗均发生了变化。此外,有4名患者(2.7%; 95%置信区间,0.1%至5.3%)在药剂师通知时已经出现了DDI的临床后果。84例患者(56.4%;95%置信区间,48.4%至64.4%)报告联合使用了草药补充剂,并检测到122种可能的HDIs。两种或以上药物的联合使用与临床上显着的DDI(优势比,2.53;95%置信区间,1.08 至5.91;P =0.03)的高风险相关。
在这项前瞻性研究中经常发现潜在的临床相关性DDI和可能的HDIs。需要采用多学科的方法来确定和避免与抗癌治疗有潜在危害的组合。
原文出处:Allan Ramos-Esquivel,et.al. Potential Drug-Drug and Herb-Drug Interactions in Patients With Cancer: A Prospective Study of Medication Surveillance .Journal of Oncology Practice. 2017.
此文系梅斯医学(MedSci)原创整理编译,转载须授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#相互作用#
39
#前瞻性研究#
28
#practice#
44
#前瞻性#
27
#Oncology#
24
#Oncol#
32
#癌症患者#
32
#互作#
28
#联合用药#
33
学习了,谢谢分享
87