BMJ:左外踝巨大渗出性包块病例报道
2015-11-07 seven L 译 MedSci原创
61岁精神分裂症男性,以发烧、疲劳、腿部疼痛和行走困难为主要表现。在他的腿和手肘有质硬包块,最大的位于左外踝(直径14cm),且有开放性创口,持续渗出。X线:病变区域有软组织包块和多个钙化灶。渗出物含有针状晶体,该物质见于痛风石。患者最初的尿酸值为494 µmol/L。患者停止服用治疗高尿酸血症的药物:苯溴马隆和柠檬酸钾;开始口服别嘌呤醇、栓剂双氯芬酸、静注盐酸头孢替安。原始出处:Tomohiko
61岁精神分裂症男性,以发烧、疲劳、腿部疼痛和行走困难为主要表现。
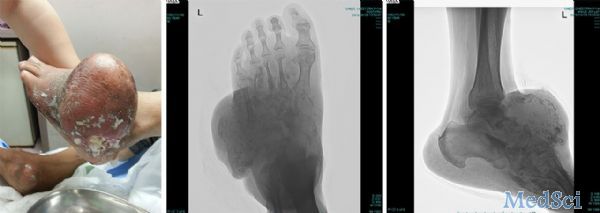
在他的腿和手肘有质硬包块,最大的位于左外踝(直径14cm),且有开放性创口,持续渗出。
X线:病变区域有软组织包块和多个钙化灶。
渗出物含有针状晶体,该物质见于痛风石。
患者最初的尿酸值为494 µmol/L。
患者停止服用治疗高尿酸血症的药物:苯溴马隆和柠檬酸钾;开始口服别嘌呤醇、栓剂双氯芬酸、静注盐酸头孢替安。
原始出处:
Tomohiko Sato.Giant exudative masses of major joints.BMJ 2015;351:h5178
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习了
55
#包块#
58
#BMJ#
24