Immunity:复旦中山医院武多娇副研究员发表Ⅰ型干扰素的免疫代谢作用
2016-06-29 MedSci MedSci原创
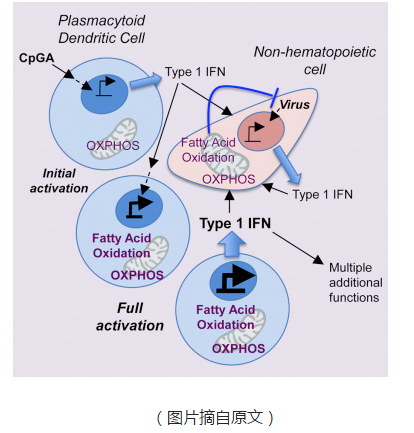
2016年6月21日,国际免疫学权威刊物《Immunity》在线发表了复旦大学附属中山医院武多娇副研究员为第一作者的一篇研究论文,研究发现Ⅰ型干扰素(IFNs)可促进浆细胞样树突状细胞(pDCs)的脂肪酸氧化(FAO)增强,这一作用是支持pDCs快速激活及发挥分泌功能的关键;而且该代谢调节作用是Ⅰ型IFNs发挥免疫功能抑制病毒复制的重要机制之一。该论文被置于Immunity杂志网站首页推荐并配有行
2016年6月21日,国际免疫学权威刊物Immunity在线发表了复旦大学附属中山医院武多娇副研究员为第一作者的一篇研究论文,研究发现Ⅰ型干扰素(IFNs)可促进浆细胞样树突状细胞(pDCs)的脂肪酸氧化(FAO)增强,这一作用是支持pDCs快速激活及发挥分泌功能的关键;而且该代谢调节作用是Ⅰ型IFNs发挥免疫功能抑制病毒复制的重要机制之一。该论文被置于Immunity杂志网站首页推荐并配有行业专家评述。

(图中上左一为武多娇副研究员)
IFNs是一组机体宿主细胞应答病毒、细菌、寄生虫及肿瘤细胞等感染或刺激,分泌的重要的具有多种功能的细胞因子。它们具有广谱抗病毒,调节细胞生长分化及免疫功能等多种生物活性。IFNs家族主要包括三类—Ⅰ、Ⅱ、Ⅲ型干扰素;其中Ⅰ型IFNs(主要是IFNα和IFNβ)具有突出的抗病毒感染和免疫调节作用,因此备受关注。
免疫代谢(immunemetabolism)是近5年新兴的领域,人们认识到细胞外信号诱导免疫细胞成熟的关键步骤就是它们细胞代谢的重组。细胞代谢重组(metabolic reprogramming)是免疫细胞执行特定功能的基础,调控细胞代谢是机体固有性和适应性免疫反应的重要机制之一。免疫细胞通常缺乏营养储备,而对于各种生物来说,免疫系统持续感应和应对外界环境的威胁,这是一个巨大的需求和消耗能量的过程。例如,固有免疫细胞或者适应性免疫细胞激活后可分泌大量细胞因子、趋化因子、炎症介质;这些免疫应答只能依赖于免疫细胞从微环境中快速吸收和利用糖、氨基酸和脂肪酸;同时,代谢中间产物参与组蛋白化学修饰,改变染色质构象,发挥转录调节作用。
浆细胞样树突状细胞(pDCs)是一类以大量分泌Ⅰ型IFNs为突出特征的树突状细胞亚群,它的细胞形态、功能与GM-CSF诱导分化的DCs或传统DCs(cDCs)相比有显著差异,在机体抵御病毒感染中起到重要作用。武博士及同事发现Ⅰ型IFNs具有诱导细胞代谢重组的功能。该研究发现伴随pDCs活化,pDCs的FAO水平显著增强。细胞能量代谢实时监测发现,活化的细胞中反映FAO的指标—耗氧率(OCR)和呼吸储备能力(SRC)明显升高;而阻断FAO通路可显著抑制pDCs分泌细胞因子以及细胞表面共刺激分子的表达,同时抑制细胞活化伴随升高的脂肪酸氧化水平。
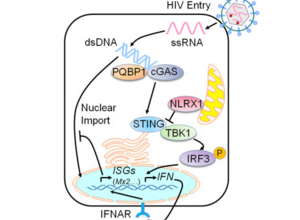
IFNs通过诱导细胞表达多种蛋白质而发挥生物学功能,表达这些功能蛋白质的基因称作干扰素刺激基因(ISGs)。武博士及同事应用IFNAR基因敲除小鼠及RNAseq技术检测分析发现I型IFNs通过I型IFNs受体介导自分泌信号促进pDCs的FAO和OXPHOS。ISGs中有大量的代谢调节相关基因参与了Ⅰ型IFNs介导的细胞代谢重组作用。该研究在体内淋巴细胞脉络丛脑膜炎病毒(LCMV)感染的小鼠模型中发现抑制FAO将促进LCMV病毒复制,说明Ⅰ型IFNs促进LCMV感染小鼠体内能量分解代谢,竞争性抑制病毒复制活动,是其发挥抗病毒感染的重要机制之一。
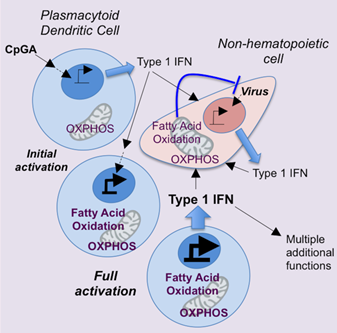
杂志社在发表该研究成果时,配发l篇评述“pDCs Take a Deep Breath to Fight
Viruses”。该评述指出深入理解免疫代谢调控机制可为我们提供防治疾病新的视野和手段。Ⅰ型IFNs为重要的抗感染、肿瘤或者炎症的细胞因子,具有复杂的免疫调节功能。免疫系统抵御病原微生物保持机体内环境稳态。这些功能需要足够的能量支持及精准细胞代谢通路的控制。此研究从免疫代谢角度阐明Ⅰ型IFNs新的抗病毒机制;并且也通过解析Ⅰ型IFNs对于靶细胞的免疫代谢调节分子机制,揭示操纵免疫代谢途径的可能性。
原始出处:
Wu D, Sanin DE,et al.Type 1 Interferons Induce Changes in Core Metabolism that Are Critical for Immune Function.Immunity. 2016 Jun 21;44(6):1325-36.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Immunity#
0
己拜读,受益匪浅
71
#研究员#
0
#复旦中山医院#
30
#I型干扰素#
42
#中山医院#
31
#复旦#
33