J Rheumatol:脊柱关节炎患者10年TNFi药物生存率的比较分析及预测因素
2018-06-23 Rheum情报官 Rheum情报官
脊柱关节炎(SpA)的治疗随着生物制剂的应用发生了巨大改变。针对SpA的大多数研究重点关注于其临床亚型,主要是强直性脊柱炎(AS)和银屑病关节炎(PsA)。目前仅有少数在肿瘤坏死因子抑制剂(TNFi)应用早期开展的短期随访研究评估了TNFi在SpA总体及不同亚型患者中的应用。然而,短期治疗结局报告对于SpA至关重要,但仍存在一定的缺陷。因此,Flouri ID等研究者于2018年6月份在Journ
脊柱关节炎(SpA)的治疗随着生物制剂的应用发生了巨大改变。针对SpA的大多数研究重点关注于其临床亚型,主要是强直性脊柱炎(AS)和银屑病关节炎(PsA)。目前仅有少数在肿瘤坏死因子抑制剂(TNFi)应用早期开展的短期随访研究评估了TNFi在SpA总体及不同亚型患者中的应用。然而,短期治疗结局报告对于SpA至关重要,但仍存在一定的缺陷。因此,Flouri ID等研究者于2018年6月份在Journal of Rheumatology上发表了一篇文章,旨在评估接受TNFI首次治疗的SpA总体及不同亚型患者的10年药物生存率,并确定药物保留的预测因子。
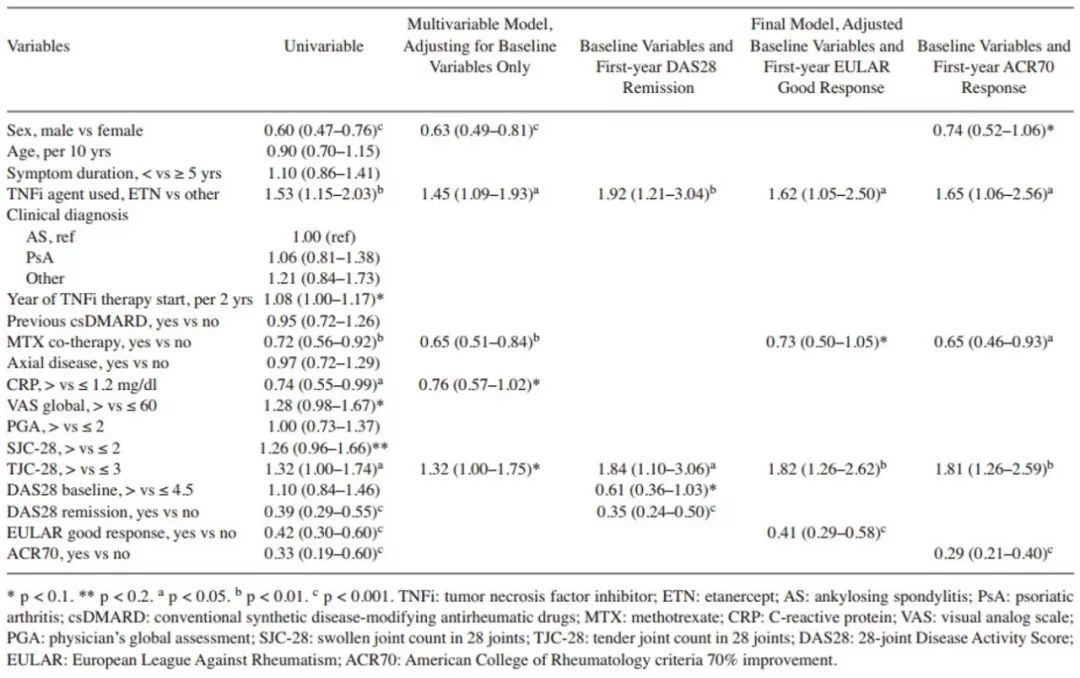
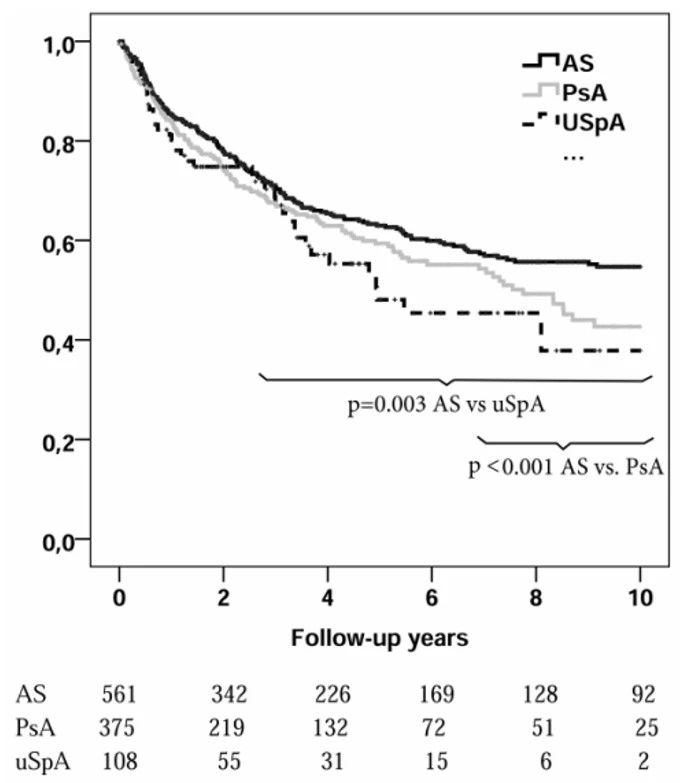
这是一项前瞻性、多中心、观察性队列研究,纳入希腊生物治疗登记中2004-2014年间首次使用TNFi的SpA患者1077例,使用Kaplan-Meier曲线和Cox回归模型进行分析。分析结果显示,404例(37.5%)患者停止治疗(随访4288患者-年)。10年药物生存率为49%。在未调整分析中,AS患者的TNFi生存率较未分化SpA患者和PsA患者高,其中在最初2.5年和7年显著更高(P值分别为0.003和<0.001),且孤立的中轴型关节炎高于外周型关节炎(P= 0.001)(图1 &图2)。在所有多变量分析中,男性是TNFi生存时间较长的预测因子。使用甲氨蝶呤(MTX)是PsA和外周型关节炎的预测因子。由于无效率较低,不存在外周型关节炎和使用单克隆抗体(与非抗体TNFi相反)是中轴型关节炎患者TNFi存活时间更长的独立预测因子。中轴型或外周型关节炎患者在第1年达到主要应答是较长治疗保留时间的最强预测因子(强直性脊柱炎疾病活动评分无活动性病变:HR =0.33,95%CI:0.26-0.41;28关节疾病活动评分缓解:HR= 0.35,95%CI:0.24-0.50)(表1 &表2)。该研究局限性在于没有关节外活动的相关数据(附着点炎、趾炎、银屑病或IBD相关复发),这可能会影响医师制定治疗决策;此外,根据风湿病专家的诊断而不是分类标准诊断进行患者招募,这可能是大多数登记研究固有的局限性。
图1. 不同临床诊断患者类型的TNFi生存率
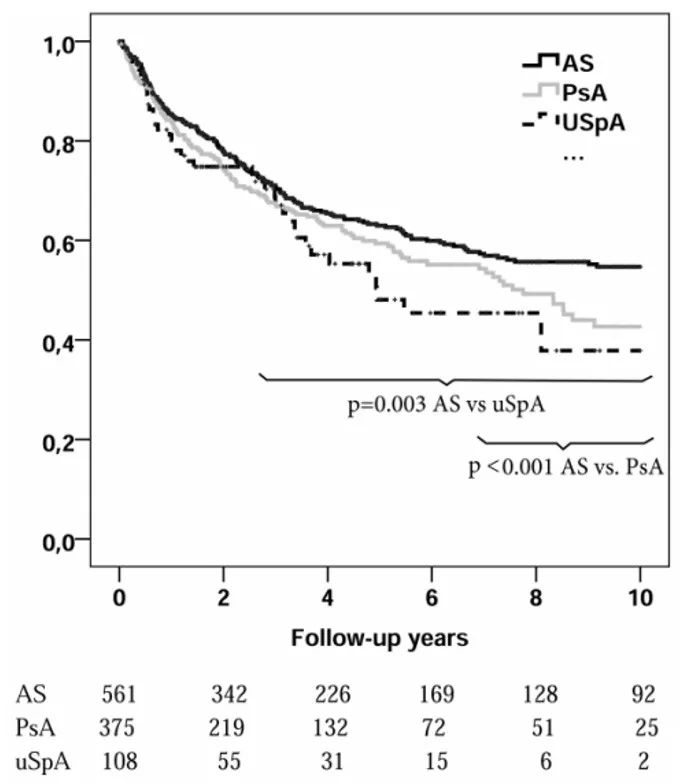
图2. 不同关节受累患者的TNFi生存率
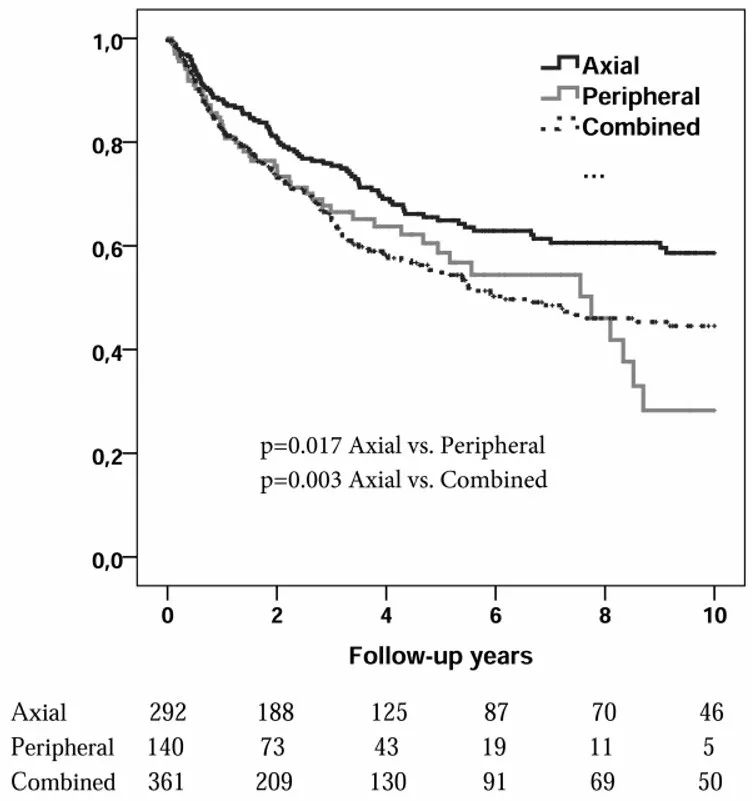
表1. 中轴型炎症性关节炎患者中TNFi停药预测因素的Cox回归分析
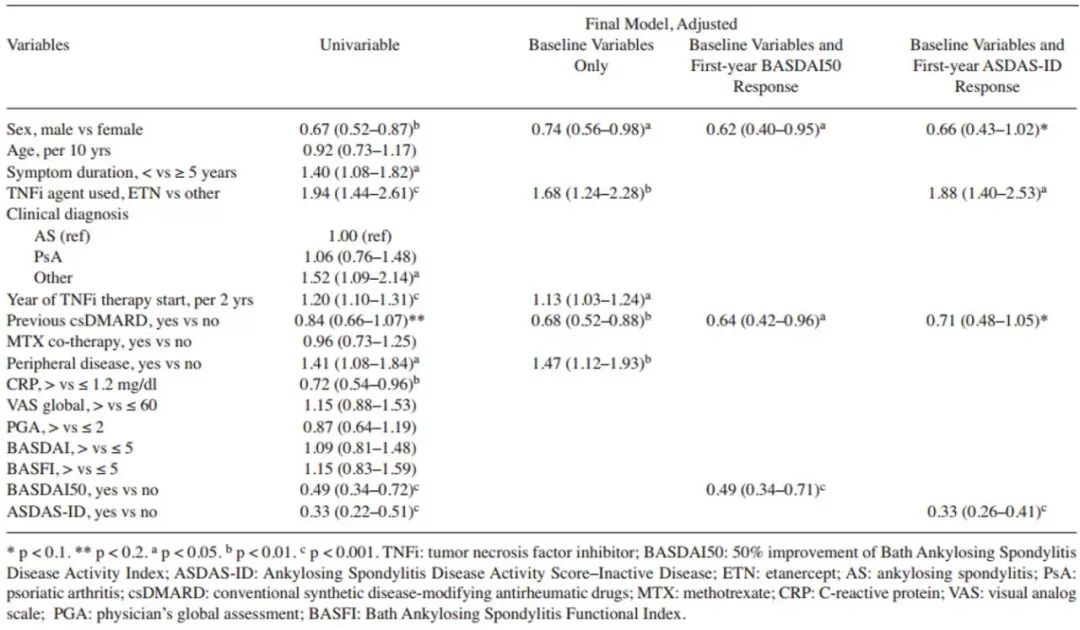
表2. 外周型关节炎患者中TNFi停药预测因素的Cox回归分析
总之,SpA患者首次使用TNFi的长期保留率高,尤其是中轴型病变的男性。TNFi长期生存的最强预测因子是治疗第1年内的主要应答结果。
原始出处:
Flouri ID, Markatseli TE, Boki KA, Papadopoulos I, Skopouli FN, Voulgari PV, Settas L, Zisopoulos D, Iliopoulos A, Geborek P, Drosos AA, Boumpas DT, Sidiropoulos P. Comparative Analysis and Predictors of 10-year Tumor Necrosis Factor Inhibitors Drug Survival in Patients with Spondyloarthritis: First-year Response Predicts Longterm Drug Persistence. J Rheumatol. 2018 Jun;45(6):785-794. doi: 10.3899/jrheum.170477. Epub 2018 Apr 1.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#药物生存率#
25
#比较分析#
29
#生存率#
18
#预测因素#
27
#关节炎#
18
#脊柱关节炎#
18
#TNF#
20
#TNFi#
27