Diabetes Care:青年2型糖尿病患者较1型有更高的长期并发症及致死风险
2013-07-29 Diabetes Care dxy
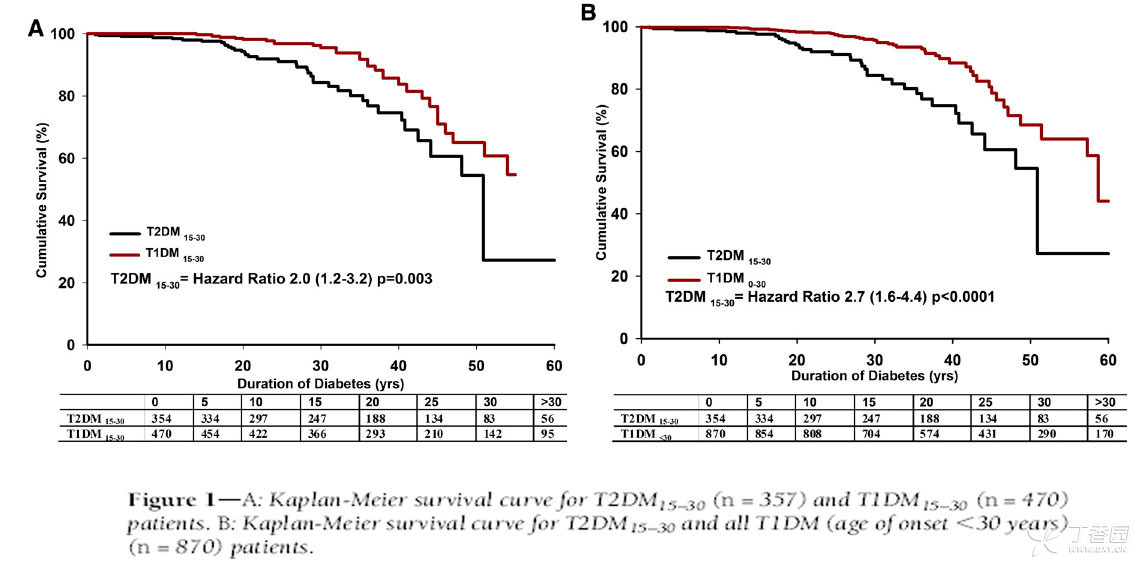
代谢组学T2DM和T1DM患者累积存活率 为了评价青年2型糖尿病(T2DM)患者的长期临床结局和存活率,并将其与具有相似发病年龄的1型糖尿病(T1DM)患者进行比较,来自澳大利亚皇家阿尔弗雷德王子医院糖尿病中心的Constantino等进行了一项研究,研究发现,与T1DM比较,青年T2DM是更致命的糖尿病表型,具有较高的死亡率、更多的糖尿病并发症和不良心血管疾病危险因素。研究结果在线发表于201
代谢组学T2DM和T1DM患者累积存活率
为了评价青年2型糖尿病(T2DM)患者的长期临床结局和存活率,并将其与具有相似发病年龄的1型糖尿病(T1DM)患者进行比较,来自澳大利亚皇家阿尔弗雷德王子医院糖尿病中心的Constantino等进行了一项研究,研究发现,与T1DM比较,青年T2DM是更致命的糖尿病表型,具有较高的死亡率、更多的糖尿病并发症和不良心血管疾病危险因素。研究结果在线发表于2013年7月11日的美国《糖尿病治疗》(Diabetes Care)杂志上。
患者记录来自1986年皇家阿尔弗雷德王子医院建立的糖尿病临床数据库,将病人数据与澳大利亚国家死亡指数匹配,以明确至2011年6月所有受试者的死亡结局。从多个方面对354名发病年龄在15-30岁的T2DM患者(T2DM15-30)和T1DM患者的临床和死亡结局进行比较,然而主要与470名与T2DM患者有相似发病年龄的T1DM受试者(T1DM15-30)比较,这样使得年龄对结局的混杂影响减少到最低程度。
对T2DM和T1DM两组患者的中位观察时间分别为21.4年和23.4年,结果显示,824名患者有71例死亡,死亡率为8.6%。T2DM15-30组死亡率明显增多,死亡风险增高(HR 2.0),出现死亡时病程明显较短,年龄相对较年轻。T2DM15-30组心血管疾病死亡人数较多。T2DM和T1DM组比较,尽管血糖控制情况和病程相当,T2DM15-30组蛋白尿发生率和不良的心血管危险因素较高,甚至出现在糖尿病发病后不久。T2DM15-30组神经病变评分和大血管并发症也升高(P<0.0001)。
研究发现,与T1DM比较,青年T2DM是更致命的糖尿病表型,具有较高的死亡率及更多的糖尿病并发症和不良心血管疾病风险。

Constantino MI, Molyneaux L, Limacher-Gisler F, Al-Saeed A, Luo C, Wu T, Twigg SM, Yue DK, Wong J.Long-Term Complications and Mortality in Young-Onset Diabetes: Type 2 diabetes is more hazardous and lethal than type 1 diabetes.Diabetes Care. 2013 Jul 11. [Epub ahead of print]
- PMID:
- 23846814
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Diabetes#
31
#BET#
29
#并发#
28
#DIA#
26
#2型糖尿病患者#
30
#糖尿病患者#
27