JCEM:C反应蛋白与2型糖尿病发病率关联的种族差异
2022-02-10 MedSci原创 MedSci原创
较高的C反应蛋白水平是糖尿病发病的危险因素,但黑人成人糖尿病的过度负担仅见于C反应蛋白较低的人群,这表明炎症不太可能是这种种族差异的主要驱动因素。
炎症与男性和女性患糖尿病的风险增加有关,与白人成年人相比,黑人成人的炎症生物标志物显著升高,包括C反应蛋白。较高的炎症标志物也与糖尿病的危险因素有关,包括年龄、人口统计学、人体测量学、饮食、生活方式、社区和心理社会因素,表明炎症可能介导了这些风险因素与糖尿病发病率之间的因果关系。

尽管炎症标志物与糖尿病发病风险相关,但炎症对糖尿病发病的种族差异的影响尚未明确。近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,研究人员旨在评估C反应蛋白是否介导了黑人和白人糖尿病发病率的差异。
卒中地理和种族差异原因(REGARDS)研究在2003-2007年期间招募了30239名年龄≥45岁的美国黑人和白人成人,大约10年后进行了第二次随访。在没有基线糖尿病的参与者中,研究人员使用改进的泊松回归计算了在第二次就诊时按C反应蛋白水平调整的性别和种族分层风险比(RR)。反向优势加权估计了C反应蛋白对种族差异的介导百分比。
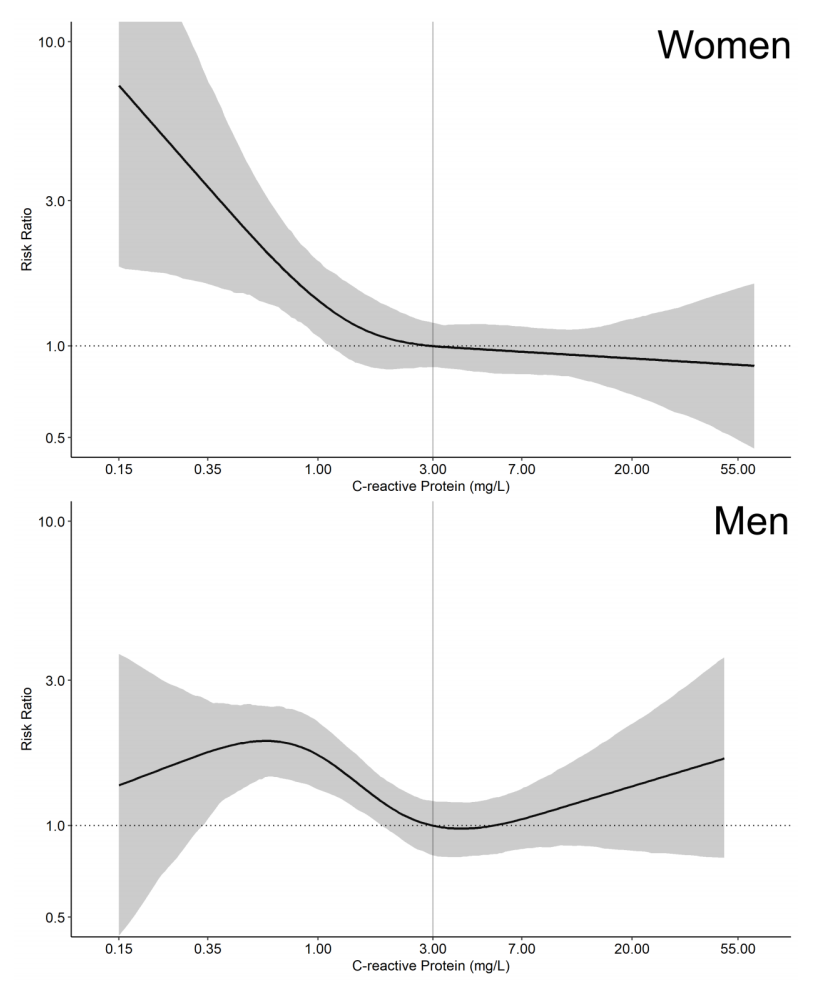
在基线没有糖尿病的11073名参与者(33%为黑人,67%为白人)中,1389人(12.5%)患上了糖尿病。与白人参与者相比,黑人参与者的基线C反应蛋白水平更高,糖尿病发病率更高。相对于C反应蛋白<3mg/L,C反应蛋白≥3mg/L与所有种族-性别分层的糖尿病风险增加相关。黑人参与者在C反应蛋白<3mg/L时患糖尿病的风险较高,但在C反应蛋白≥3mg/L时则不然。在女性中,C反应蛋白介导了10.0%的糖尿病发病的种族差异。这种介导效应在男性受试者中并未观察到。
由此可见,较高的C反应蛋白水平是糖尿病发病的危险因素,但黑人成人糖尿病的过度负担仅见于C反应蛋白较低的人群,这表明炎症不太可能是这种种族差异的主要驱动因素。
原始出处:
Kaitlyn M. Peper.et al.C-reactive protein and racial differences in type 2 diabetes incidence: The REGARDS study.JCEM.2022.https://academic.oup.com/jcem/advance-article/doi/10.1210/clinem/dgac074/6524616
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JCE#
36
#发病率#
32
#JCEM#
38
#C反应蛋白#
46
#种族差异#
0
不错的文章
58