Science子刊:新技术让骨髓移植病人不再受到化疗伤害
2016-08-13 佚名 生物谷
造血干细胞移植也即骨髓移植是一种强大的技术,能够为病人提供终生治愈多种疾病的希望。但是这种技术具有很大毒性,目前只用于治疗一些病情最严重的病人。现在来自美国斯坦福大学医学院的研究人员在小鼠上开发出一种进行骨髓移植的新方法,可以大大降低毒性。相关研究结果发表在国际学术期刊Science Translational Medicine上。有毒的治疗为了成功地进行造血干细胞移植,首先必须通过化疗或放疗杀死

造血干细胞移植也即骨髓移植是一种强大的技术,能够为病人提供终生治愈多种疾病的希望。但是这种技术具有很大毒性,目前只用于治疗一些病情最严重的病人。现在来自美国斯坦福大学医学院的研究人员在小鼠上开发出一种进行骨髓移植的新方法,可以大大降低毒性。
相关研究结果发表在国际学术期刊Science Translational Medicine上。
有毒的治疗
为了成功地进行造血干细胞移植,首先必须通过化疗或放疗杀死病人自身的造血干细胞,这样的治疗具有很大的毒性足以对多种器官造成严重损伤,严重者甚至发生死亡。基于这些原因,只有当疾病的风险高于移植本身风险的时候才会进行造血干细胞移植。
为了避免这些严重的副作用,斯坦福的研究人员开发了一系列生物学方法能够为造血干细胞移植清除障碍,不需要使用化疗或放疗。
使用抗体
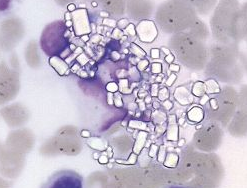
科学家们首先使用了一种能够与造血干细胞表面主要标记物c-kit结合的抗体。这种抗体与c-kit结合会导致免疫缺陷小鼠的造血干细胞被清除。但是这种抗体不能够有效地应用在存在免疫功能的受体上。研究人员为了增强抗体的作用,将其与其他抗体联合使用,同时阻断细胞表面蛋白CD47。阻断CD47能够让巨噬细胞“吃掉”这些被c-kit抗体覆盖的靶细胞。
随着CD47被阻断,再结合c-kit抗体的作用,免疫系统能够有效清除受体小鼠体内的造血干细胞,为造血干细胞移植移除障碍,帮助供体造血干细胞驻留在受体骨髓中,帮助受体形成新的血液和免疫系统。
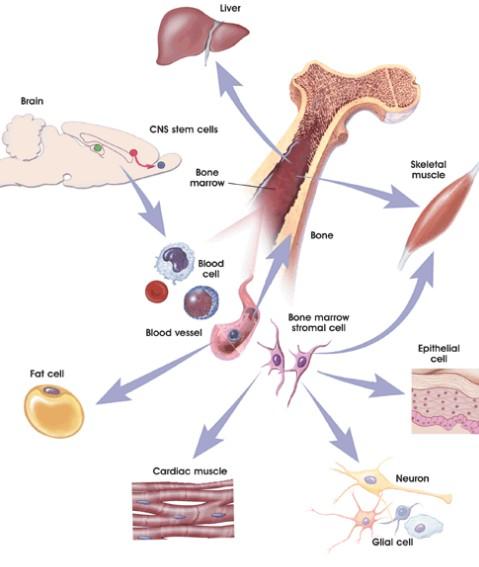
由于供体提供的骨髓不仅包含造血干细胞其中还有供体的免疫细胞,会对受体组织造成损伤。因此研究团队进一步纯化了供体的骨髓,只包含造血干细胞不包含可能造成受体组织损伤的免疫细胞。
这些技术在小鼠模型上的成功燃起了该技术在人体内获得成功的希望。如果该方法最终被证明对人类既安全又有效,那将有望用于治疗自身免疫疾病,先天性代谢疾病以及一些癌症,同时还可以让器官移植更安全成功率更高。
原始出处
Akanksha Chhabra1,*, Aaron M. Ring2,3,4,*, Kipp Weiskopf2,3,4,*, Peter John Schnorr1, Sydney Gordon2,3,4, Alan C. Le1, Hye-Sook Kwon1, Nan Guo Ring2,3,4, Jens Volkmer2,3,4, Po Yi Ho2,3,4, Serena Tseng2,3,4, Irving L. Weissman2,3,4,5 and Judith A. Shizuru.Hematopoietic stem cell transplantation in immunocompetent hosts without radiation or chemotherapy.Science Translational Medicine.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#新技术#
26
好好学习一下
60
#SCIE#
34
继续学习
48
继续关注
62
内容丰富
59
期待临床使用
64
期待尽快运用到临床!
18
继续关注
20
继续学习
16