Hypertension:颈动脉粥样硬化斑块和血清尿酸与脑血管事件相关
2022-06-09 MedSci原创 MedSci原创
目前的研究支持尿酸在颈动脉粥样硬化发病机制中作为一个潜在的组织参与分子和全身性生物标志物的潜在作用。尿酸可能为斑块不稳定性和随后的缺血性脑血管事件提供一种解释机制。
缺血性脑卒中是世界范围内发病率和死亡率的主要原因之一。但是目前颈动脉斑块内尿酸浓度及其与脑血管事件之间的关系尚未被评估或量化。血清尿酸是全身炎症的标志,也是动脉粥样硬化的危险因素。然而,其与颈动脉斑块不稳定和卒中发病机制的关系也并不明确。
近日,心血管权威杂志Hypertension上发表了一篇研究文章,在接受颈动脉内膜切除术的患者中,研究人员的目的是确定有症状与无症状颈动脉斑块中尿酸含量是否存在差异,以及血清尿酸是否与脑血管症状(卒中、短暂性缺血发作或眩晕)相关。
研究人员在受试者进行颈动脉内膜切除术时收集了颈动脉粥样硬化斑块数据,并采用格莫里甲基苯丙胺银染色和抗尿酸免疫组化染色评估了尿酸的情况,并采用酶比色法测定了尿酸的含量。临床资料是通过回顾性审查来获得的。
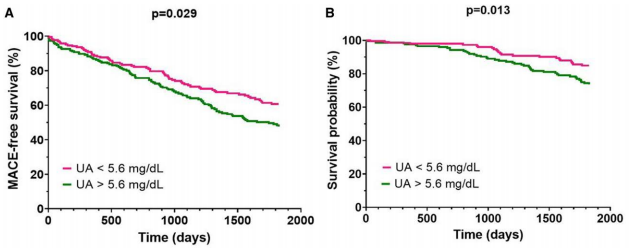
研究人员采用格莫里甲基苯丙胺银染色(20[86.9%] vs. 2[22.2%];P=0.001)和抗尿酸免疫组化(16例[69.5%] vs. 1例[11.1%];P=0.004)在有症状斑块(n=23)和无症状斑块(n=9)的颈动脉斑块中检测到了尿酸存在。有症状斑块中尿酸浓度高于无症状斑块(25.1[9.5] vs. 17.9[3.8]µg/g;P=0.021)。颈动脉内膜切除术前,有症状患者(n=341)的血清尿酸水平高于无症状患者(n=146)(5.9[四分位数范围为4.6-6.9]mg/dL vs. 5.2[四分位数范围为4.6-6.2]mg/dL;P=0.009)。
由此可见,目前的研究支持尿酸在颈动脉粥样硬化发病机制中作为一个潜在的组织参与分子和全身性生物标志物的潜在作用。尿酸可能为斑块不稳定性和随后的缺血性脑血管事件提供一种解释机制。
原始出处:
Valentina Nardi.et al.Uric Acid Expression in Carotid Atherosclerotic Plaque and Serum Uric Acid Are Associated With Cerebrovascular Events.Hypertension.2022.https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.122.19247
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#TENS#
44
#颈动脉#
45
#粥样硬化#
52
#PE#
45
#血管事件#
44
#斑块#
32
#颈动脉粥样硬化#
39
#血清尿酸#
42
#Hypertension#
44
#动脉粥样硬化斑块#
38