JAHA:疑似或已知冠状动脉疾病患者VEGF-C水平与死亡率
2018-10-27 xing.T MedSci原创
由此可见,在疑似或已知冠状动脉疾病的患者中,低VEGF-C水平可独立预测全因死亡率。
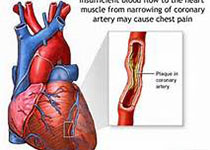
已经有研究人员提出淋巴系统在胆固醇代谢和心血管疾病中起重要作用。然而,血管内皮生长因子-C(VEGF-C)(淋巴管生成的主要参与者)与疑似或已知冠状动脉疾病患者的死亡率和心血管事件的关系尚不清楚。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员对2418名疑似或已知冠状动脉疾病患者进行了一项多中心前瞻性队列研究,该患者接受了选择性冠状动脉造影。主要预测因子是血清VEGF-C水平。主要结局是全因死亡。次要结局是心血管死亡,主要不良心血管事件定义为心血管死亡、非致命性心肌梗死和非致命性卒中的复合事件。
在3年的随访期间,254名患者死于任何原因,88名死于心血管疾病,165名患者发生了重大不良心血管事件。调整已知的危险因素后,VEGF-C水平与全因死亡(每增加1-SD的风险比为0.69; 95%置信区间为0.60-0.80)和心血管死亡(风险比为0.67; 95%置信区间为0.53-0.87)呈显著的负相关,但与主要不良心血管事件无关(风险比为0.85; 95%置信区间为0.72-1.01)。即使将N末端脑钠尿肽、敏感性心肌肌钙蛋白-I和高敏C-反应蛋白加入到已知的危险因素的模型后,VEGF-C水平的加入进一步改善了对全因死亡的预测,但不是心血管死亡或主要不良心血管事件。在1717名疑似冠状动脉疾病患者中观察到一致的结果。
由此可见,在疑似或已知冠状动脉疾病的患者中,低VEGF-C水平可独立预测全因死亡率。
原始出处:
Hiromichi Wada.et al.VEGF‐C and Mortality in Patients With Suspected or Known Coronary Artery Disease.JAHA.2018. https://www.ahajournals.org/doi/10.1161/JAHA.118.010355
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#疾病患者#
44
#冠状动脉疾病#
32
#AHA#
30
#VEGF#
34