Eur Radiol:胸部CT读片,有啥好办法提高检出以磨玻璃影为主肺癌的正确率呢?
2017-12-12 shaosai MedSci原创
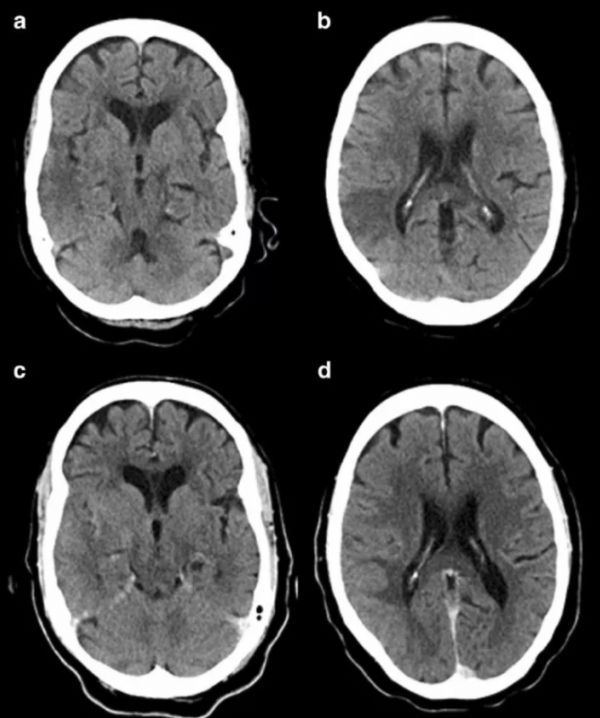
本研究旨在评估CT时间剪影(TS)方法在检出以磨玻璃影为主肺癌(LC-pGGO)的价值,并将结果发表在Eur Radiol上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#磨玻璃影#
44
是一项什么Ct技术
74
#胸部CT#
48
学习了受益匪浅
72
学习一下谢谢
77