Ann Intern Med:轻度原发性甲状旁腺功能亢进的死亡率和发病率
2022-04-23 MedSci原创 MedSci原创
甲状旁腺切除术似乎不能降低轻度PHPT患者的发病率或死亡率。因此,在至少10年的时间里,该研究没有观察到与死亡、骨折、癌症、心脑血管事件或肾脏发病率相关的不良影响的证据。
原发性甲状旁腺功能亢进(PHPT)是一种常见的内分泌疾病,与骨折、心血管疾病、肾脏疾病和癌症的风险增加和死亡率增加有关。对于轻度PHPT伴轻度高钙血症且无已知发病率的患者,甲状旁腺切除术(PTX)仍存在争议,因为没有进行长期随机试验。

近日,内科学权威杂志Annals of Internal Medicine上发表了一篇研究文章,该研究旨在探究PTX对轻度PHPT在死亡率(主要终点)和关键发病率(次要终点)方面的影响。
该前瞻性随机对照试验(ClinicalTrials.gov: NCT00522028)是在8个斯堪的纳维亚转诊中心内完成的。受试者为1998年到2005年期间纳入的191例轻度PHPT患者。其中,95例患者随机分为PTX组,96例分为无干预观察组(OBS)。研究人员从瑞典和挪威死亡原因登记处获取了受试者死亡日期和原因,随机分组10年后,并经过持续到2018年的延长观察期。每年对发病率事件进行前瞻性记录。
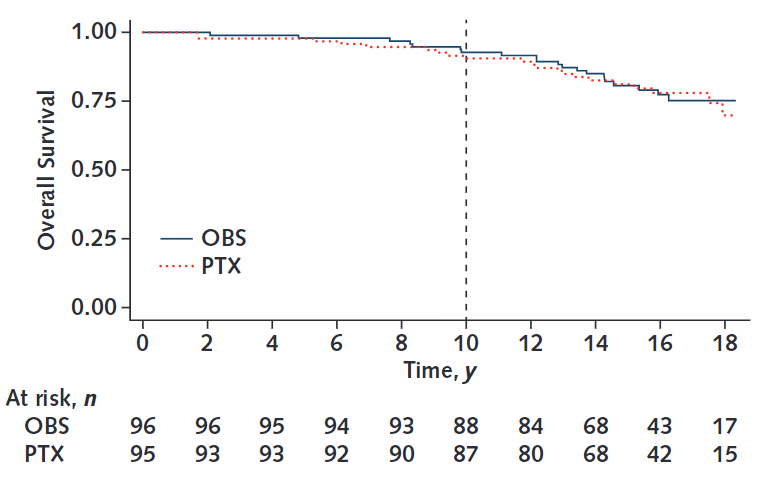
10年后,15例患者死亡(PTX组8例,OBS组7例)。在延长的观察期内,发生了44例死亡,平均分布在两组之间(PTX组24例,OBS组20例)。共有101个发病率事件(心血管事件、脑血管事件、癌症、周围骨折和肾结石)在组间分布相似(PTX组52人,OBS组49人)。在研究过程中,14例患者共发生16例椎体骨折(每组7例)。
由此可见,甲状旁腺切除术似乎不能降低轻度PHPT患者的发病率或死亡率。因此,在至少10年的时间里,该研究没有观察到与死亡、骨折、癌症、心脑血管事件或肾脏发病率相关的不良影响的证据。
原始出处:
Mikkel Pretorius,et al. Mortality and Morbidity in Mild Primary Hyperparathyroidism:Results From a 10-Year Prospective Randomized Controlled Trial ofParathyroidectomy Versus Observation.Ann Intern Med 2022.https://www.acpjournals.org/doi/10.7326/M21-4416
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习了
25
#原发性#
46
#发病率#
32
#甲状旁腺功能亢进#
36
#甲状旁腺#
35
#原发性甲状旁腺功能亢进#
41
#Med#
27