Cardiovasc Diabetol:2型糖尿病患者血浆代谢物与亚临床动脉粥样硬化的相关性
2021-12-22 MedSci原创 MedSci原创
不同的代谢特征与亚临床冠状动脉粥样硬化显著相关。
心血管疾病(CVD)的发病率正在增加,部分原因是糖尿病的流行。因此需要新的预测工具和可修改的治疗靶点来加强风险评估和管理。糖尿病心脏研究(DHS)研究了血浆代谢物与亚临床动脉粥样硬化的相关性,该研究是一个针对2型糖尿病(T2D)进行队列研究。

该分析包括700名DHS参与者,438名非洲裔美国人(AAs)和262名欧洲裔美国人(EAs),其中冠状动脉钙化(CAC)使用心电门控ct进行评估。利用液相色谱-质谱联用的血浆代谢组学鉴定了853个已知代谢物。一个结合广义估计方程的特异性边缘模型检验了代谢物和CAC之间的关联(作为结果测量的对数转化(CAC + 1))。模型根据年龄、性别、BMI、糖尿病持续时间、血浆采集日期、血浆采集与CT检查之间的时间、低密度脂蛋白胆固醇(LDL-C)和他汀类药物使用情况进行调整。
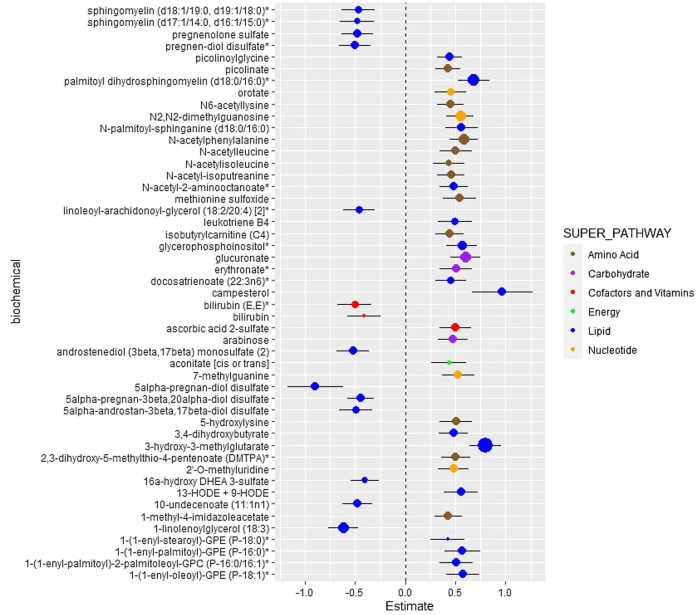
数据显示在FDR校正p值< 0.05时,AAs中有33种代谢物与CAC相关,EAs中有36种代谢物与CAC相关。雄激素、脂肪酸、磷脂酰胆碱和胆酸代谢通路与AAs中CAC相关,而脂肪酸、溶浆原和分支链氨基酸(BCAA)通路与EAs中CAC相关。

上图显示AA 中血浆代谢物与 CAC 之间的关联。该模型根据年龄、性别、BMI、吸烟状况、高血压状况、心血管疾病、糖尿病病程、血浆采集日期、血浆采集和 CT 检查之间的时间、LDL-C、他汀类药物的使用进行了调整。
上图显示了EA 中血浆代谢物与 CAC 之间的关联。该模型根据年龄、性别、BMI、吸烟状况、高血压状况、心血管疾病、糖尿病病程、血浆采集日期、血浆采集和 CT 检查之间的时间、LDL-C、他汀类药物的使用进行了调整。
综上所述,在AA和EA DHS参与者中,不同的代谢特征与亚临床冠状动脉粥样硬化显著相关。与亚临床动脉粥样硬化相关的代谢途径在患有 T2D 的 AA 和 EA 人群之间有所不同。与 AA 相比,EA 中与 CAC 显着相关的代谢物数量似乎更高。
欧洲人群的 CAC 水平远高于 AA,并且当人群之间的医疗保健可及性相同时,心肌梗塞的风险会增加。雄激素类固醇、脂肪酸和胆汁酸代谢亚途径与 AA 中的 CAC 显着相关,而雄激素类固醇、孕激素类固醇、孕烯醇酮类固醇、溶血原纤维、鞘磷脂和 BCAA 代谢亚途径与 EA 中的 CAC 相关。
参考文献:Chevli, P.A., Freedman, B.I., Hsu, FC. et al. Plasma metabolomic profiling in subclinical atherosclerosis: the Diabetes Heart Study. Cardiovasc Diabetol 20, 231 (2021). https://doi.org/10.1186/s12933-021-01419-y
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#相关性#
43
#粥样硬化#
57
#ASC#
42
#BET#
47
#代谢物#
0
#血浆代谢物#
50
#亚临床动脉粥样硬化#
55
#DIA#
45
#2型糖尿病患者#
39
#糖尿病患者#
27