J Urol:肌肉减少性肥胖对泌尿系统癌症患者预后的影响
2021-05-30 MedSci原创 MedSci原创
肌肉减少症或可预测泌尿系统癌症患者的不良预后,肌肉减少性肥胖是否也与泌尿系统癌症患者的预后相关?
肌肉减少症,是一种因持续的骨骼肌量减少、强度和功能下降而引起的综合症。骨骼肌是人体运动系统的动力,肌肉的衰老和萎缩是人体衰老的重要标志,非常容易引起骨折以及关节损伤等问题。
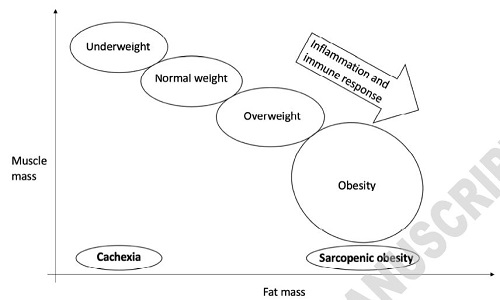
肌肉减少性肥胖(SO)是两种疾病混合的身体状态,一方面是人体脂肪含量增加,另一方面是肌肉含量减少。肌肉减少性肥胖是一个重要的公共卫生问题。
既往研究显示,肌肉减少症或可预测泌尿系统癌症患者的不良预后。但肌肉减少性肥胖的临床意义尚不明确。
最新发表了“J Urol”上的一篇文章“Sarcopenic Obesity and Its Prognostic Impact on Urologic Cancers: A Systematic Review”,系统地回顾了肌肉减少性肥胖对接受治疗的肾细胞癌、尿路上皮癌和前列腺癌患者的患病率和预后的影响。
研究人员检索了Embase、PubMed/MEDLINE和Scopus数据库,查找2010年1月-2021年2月之间发表的相关文章。主要结果是总生存期 (OS)、癌症特异性生存期 (CSS) 和无进展生存期 (PFS)。次要结果是肌肉减少性肥胖的患病率。
描述脂肪增减动态的概念模型
纳入了15项研究,共包含3866名患者。 有10项评估了生存预后的研究显示,肌肉减少性肥胖与生存之间的关联是混合的:一项研究显示肌肉减少性肥胖与OS显著相关 (HR 0.7,95% CI 0.51-0.98,p=0.04);另一项研究表明OS较短的趋势与肌肉减少性肥胖相关(p=0.05);其他研究显示,肌肉减少性肥胖是泌尿系统癌症患者CSS的不良预后因素 (HR 5.0,95% CI 1.4-16.7,p=0.01)。
此外,其他所有研究都没有证明肌肉减少性肥胖与泌尿系统癌症患者的OS、CSS和PFS的预后相关。此外,肌肉减少性肥胖在泌尿系统癌症患者中的平均发生率为27% (范围11-63)。
总而言之,既往文献对肌肉减少性肥胖的定义存在较大的异质性,而且当前相关数据有限。需要进一步研究来深入了解肥胖和肌肉减少症对泌尿系统癌症患者临床预后的影响。
原始出处:
Stangl-Kremser J,Mari A,Lai L Y et al. Sarcopenic Obesity and Its Prognostic Impact on Urologic Cancers: A Systematic Review.[J] .J Urol, 2021, undefined: 101097JU0000000000001873.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#肌肉减少#
35
#患者预后#
34
#泌尿系统癌症#
42
#癌症患者#
40
#泌尿系#
46
学习了
63
受益
57