Neurology:10年随访发现,早期降低Aβ的沉积或有助于预防阿尔茨海默病
2021-01-25 Freeman MedSci原创
10年随访发现,早期降低Aβ的沉积或有助于预防阿尔茨海默病
阿尔茨海默病(AD)的临床表现出现之前有几十年的潜伏期,此时淀粉样蛋白(Aβ)和tau蛋白聚集成病理形式很可能起了重要作用。淀粉样蛋白假说是一种广泛接受的疾病发病模型,它假设Aβ是这个病理链中最早的启动事件。
然而,许多治疗试验虽然降低了AD患者的脑Aβ,却没有产生临床改善效果,因此这一模型受到了质疑。而新的方法则建议在症状出现之前,甚至在检测到脑Aβ沉积之前,采用 "初级预防 "的方法进行抗Aβ治疗。
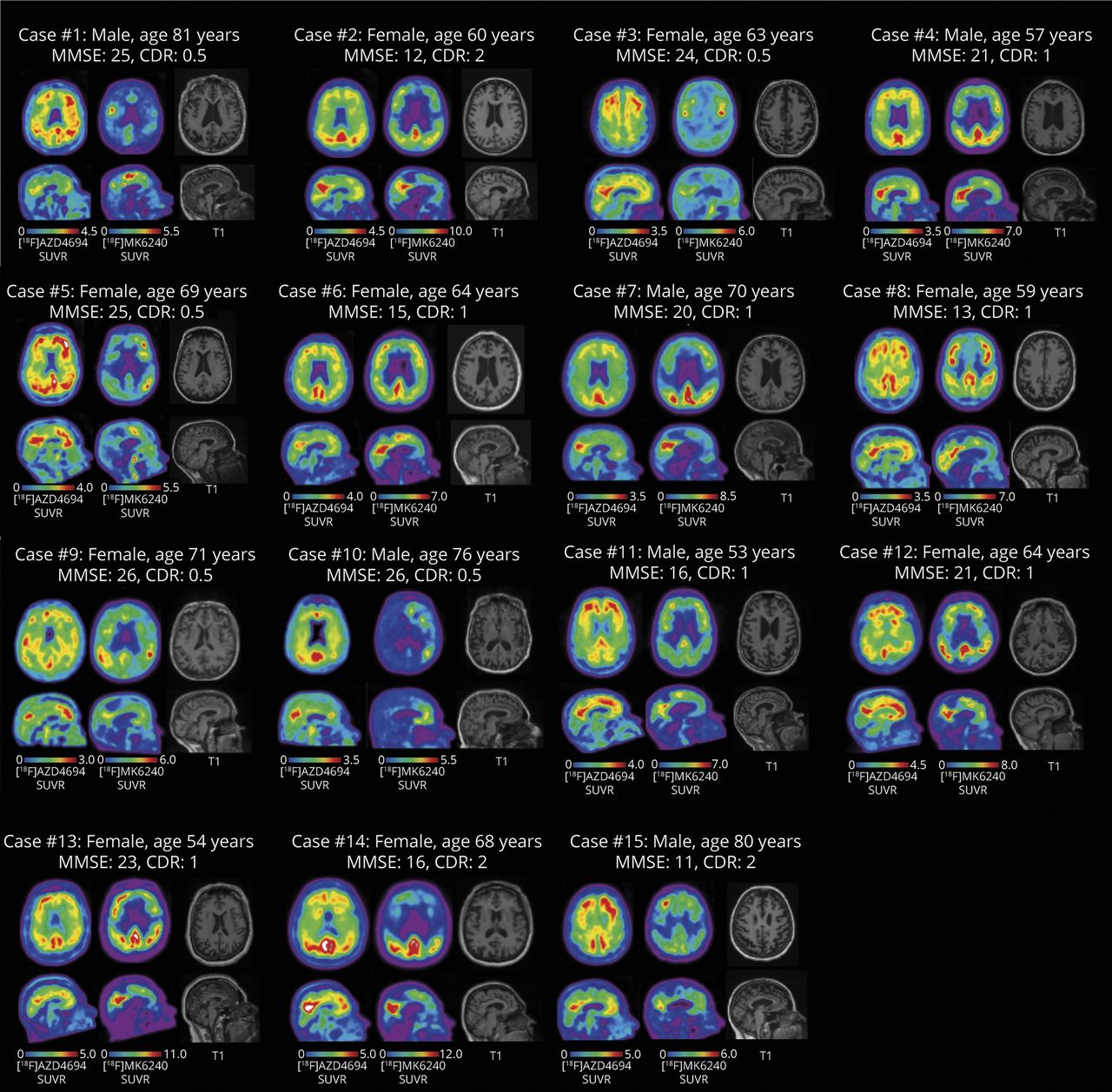
这种早期开始的治疗需要了解脑Aβ沉积的时间过程。现有的大多数淀粉样蛋白PET纵向研究受到样本量和随访时间的限制。阿尔茨海默病神经影像学计划(ADNI)于2010年开始收集连续的淀粉样蛋白[18F]-florbetapir(FBP)PET扫描,并对一些参与者持续追踪到现在。在这项研究中,他们使用了多达6次的连续FBP扫描和9年的最大随访时间来估计认知正常和损害个体的Aβ动态变化,从而去预测从认知正常到损害变化过程。
藉此,加州伯克利大学的William J Jagust等人,基于著名ADNI( Alzheimer’s Disease Neuroimaging Initiative)探究Aβ阴性的认知正常和损害者往Aβ阳性转化的时间过程和认知预后的关系。
他们采用[18F]-Florbetapir,FBP)Aβ-PET对ADNI的两个参与者样本进行研究,并跟踪长达9年。样本A包括475名认知正常(CN)老年人和轻度认知障碍(MCI)和AD患者,样本B包括220名CN Aβ-个体。藉此,样本A中FBP随时间变化的轨迹,以及样本B中Aβ PET扫描由阴性转为阳性的发生率。

结果显示。时间和脑Aβ之间的关系呈S形,从淀粉样蛋白阴性转为阳性需要6.4年,到MCI的发生又需要13.9年。
Aβ沉积率在达到阳性阈值后3.8年才开始减缓。Aβ阳性的发生率为38/1000人年,与转换(从阴性到阳性)相关的因素有年龄、基线FBP、是女性载脂蛋白E4携带者。在CN Aβ-个体中,FBP斜率与基线5年后用[18F]Flortaucipir PET测量的记忆力下降率和脑tau有关。
这个研究的重要意义在于:发现了降低脑Aβ应在AD演变的早期完成。PET扫描从Aβ-到Aβ+的过渡应该是可以预测的,因此在早期降低Aβ的进展或许能产生显著的临床效益。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#阿尔茨海#
43
#阿尔茨#
32
#Neurol#
37
#阿尔茨海默#
36
#Aβ#
29
学习
83