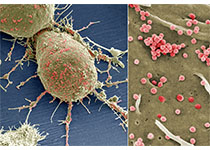
BJC近期发表了一篇文章,研究CDX2表达对II期结肠癌患者预后的影响。
研究分析了两个无偏倚的队列,代表了2002年和2003年期间在丹麦接受手术的II期结肠癌的所有患者。利用免疫组化在肿瘤切片上评估CDX2表达情况。根据结果将患者分为三组,CDX2阳性组,CDX2中度组和CDX2阴性组,用于与临床数据进行比较。研究共纳入1157名患者。研究结果表明两个队列中CDX2表达缺失和无病生存不良具有显着关系,p ?= 0.0267和0.0118。第一个队列中,CDX2表达阴性,中度和阳性组的五年无病生存率分别为66%,72%和74%,第二个队列中分别为的62%,65%和75%。两个队列数据组合后进行多重Cox回归分析证实了CDX2对无病生存的独立预后影响。
原始出处:
Torben Frøstrup Hansen, Sanne Kjær-Frifeldt, et al. Prognostic impact of CDX2 in stage II colon cancer: results from two nationwide cohorts. BJC. November 2018 doi: https://doi.org/10.1038/s41416-018-0285-5
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CDX2#
31
#患者预后#
33
学习了,谢谢分享
58
学习了,涨知识了!
60