Cell Reports:CRISPR挖出大量抗癌靶标
2016-10-24 佚名 生物通
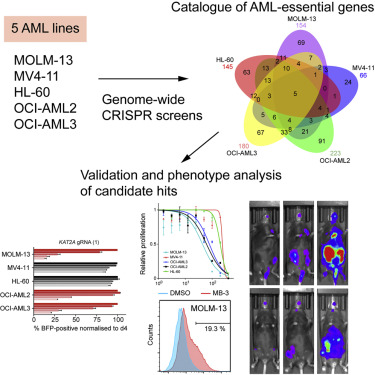
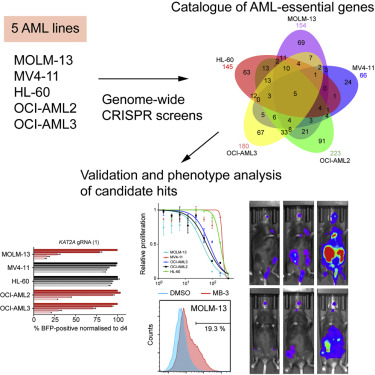
白血病是一种造血系统的恶性肿瘤,俗称“血癌”。急性髓性白血病AML是比较常见的一种白血病,现有治疗药物在临床上的效果并不理想。Wellcome Trust Sanger研究所改良了CRISPR基因编辑技术,并用该技术找到了大量治疗AML的新靶标。这项研究发表在十月十八日的Cell Reports杂志上。细菌一直在与病毒或入侵核酸进行斗争,为此它们演化出了多种防御机制,CRISPR–Cas9适应性免
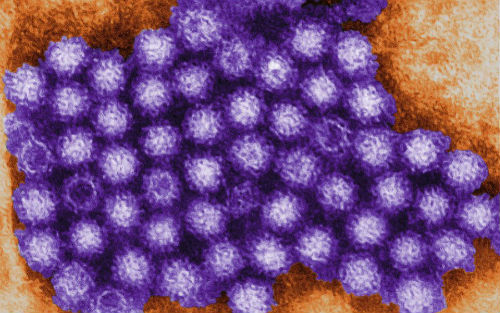
细菌一直在与病毒或入侵核酸进行斗争,为此它们演化出了多种防御机制,CRISPR–Cas9适应性免疫系统就是其中之一。规律成簇的间隔短回文重复CRISPR与内切酶Cas9的组合,可以在引导RNA的指引下,靶标并切割入侵者的遗传物质。2012年研究者们利用这一特点,将CRISPR系统制成了强大的基因组编辑工具。
研究人员改良过的CRISPR-Cas9能够有效地逐一破坏白血病细胞的所有基因。他们通过这种方式筛选癌细胞的薄弱点,寻找那些影响AML生长和生存的基因。“这是一次鉴定AML基因弱点的系统性尝试,”Sanger 研究所的Dr Kosuke Yusa说。研究显示,近五百个人类基因是白血病细胞不可或缺的,其中两百多个基因可以成为治疗靶标。这些发现为白血病药物研发带来了许多新的可能。
研究人员选择对KAT2A基因进行深入研究。他们发现,抑制KAT2A的确可以影响AML细胞的生长和生存。“KAT2A抑制对多种基因型的AML细胞都有效,这是一个令人振奋的发现,”Dr Konstantinos Tzelepis指出。进一步研究表明,在转基因小鼠的白细胞中破坏KAT2A基因可以抑制AML的发展。当KAT2A基因被破坏时,小鼠的存活期更长。
原始出处
Konstantinos Tzelepis7, Hiroko Koike-Yusa7, Etienne De Braekeleer, Yilong Li.et.al.A CRISPR Dropout Screen Identifies Genetic Vulnerabilities and Therapeutic Targets in Acute Myeloid Leukemia.Cell Reports.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Cell#
26
#CRISPR#
38
#靶标#
34
有点炫,深奥
52
这个东西也太复杂了吧
1
#CEL#
25
学习到了很多,受益匪浅
63
很有用处,了解了不少
53