颈胸段半椎体畸形伴Horner综合征2例
2019-09-27 李洋 朱泽章 史本龙 中国脊柱脊髓杂志
病例1,患者女,3岁,2011年11月15日因“先天性脊柱侧凸”入院。查体:头部向左倾斜,双侧面部发育不对称,左眼窝轻度内陷、左眼睑下垂、左眼瞳孔缩小、对光反射存在;四肢感觉及运动正常,病理征未引出。入院全脊柱X线片及三维CT示:T2、T3、T4、T5半椎体畸形伴对侧分节不良,颈胸段侧凸Cobb角77°。全脊柱MRI示无脊髓空洞、脊髓纵裂、脊髓拴系等髓内异常表现。入院诊断:(1)先天性脊柱侧凸畸形
Horner综合征又称颈交感神经麻痹综合征,是指由支配头面部的交感神经传出通路中任一部分受压损伤或中断所引起的患侧瞳孔缩小、眼球内陷、上眼睑下垂、眼裂狭小及患侧面部少汗或无汗等一系列特异性临床表现的综合征。因颈交感神经节前和节后纤维在其走行路径中与椎弓根、臂丛、肺尖、颈丛、颈总动脉、颈内动静脉和甲状腺等解剖关系密切,上述结构的疾患或损伤导致的Horner综合征在临床中约占87%。既往文献中关于Horner综合征的报道多为颈部创伤、肿瘤、颈动脉夹层以及医源性损伤如深静脉置管、颈部及纵隔肿瘤手术、臂丛麻醉、产伤等。目前,文献中少见由脊柱病变及脊柱手术等引起Horner综合征的报道,且现有报道病例主要为颈胸段后纵韧带骨化或椎间盘突出引起。值得注意的是,颈胸段椎体发育异常导致压迫颈交感神经传导通路同样可导致Horner综合征。然而,由于颈胸段半椎体发病率较低,并且儿童Horner综合征的表现常不典型,因此颈胸段椎体畸形伴发的Horner综合征常被忽视。我院曾收治2例颈胸段半椎体畸形伴发Horner综合征的病例,报道如下。
临床资料
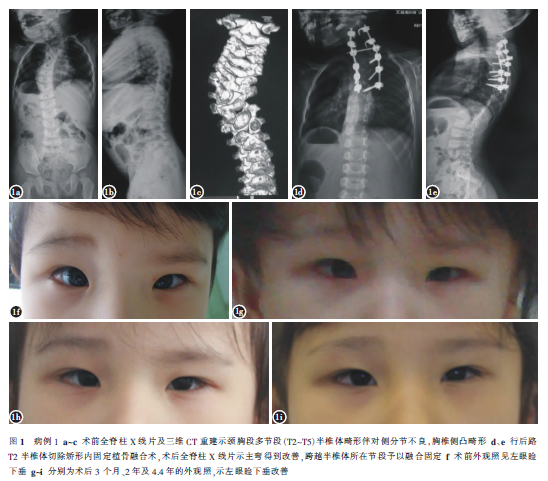
病例1,患者女,3岁,2011年11月15日因“先天性脊柱侧凸”入院。查体:头部向左倾斜,双侧面部发育不对称,左眼窝轻度内陷、左眼睑下垂、左眼瞳孔缩小、对光反射存在;四肢感觉及运动正常,病理征未引出。入院全脊柱X线片及三维CT示:T2、T3、T4、T5半椎体畸形伴对侧分节不良,颈胸段侧凸Cobb角77°。全脊柱MRI示无脊髓空洞、脊髓纵裂、脊髓拴系等髓内异常表现。入院诊断:(1)先天性脊柱侧凸畸形;(2)Horner综合征。完善入院检查后予以脊柱后路T2半椎体切除矫形内固定植骨融合术。术后3个月、1年、2年定期随访见患者左眼睑下垂有好转趋势,术后4.4年随访左眼睑下垂较术前明显改善(图1)。病例2,患者女,5岁,于2012年3月26日入院。查体:肩背部明显隆起,“剃刀背”畸形;左眼窝内陷、左眼睑下垂、左眼瞳孔缩小、对光反射存在;四肢等长,双手发育不对称,左手骨间肌、大小鱼肌肌及蚓状肌萎缩,左手指主动屈伸功能受限,前臂肌肉肌力4级,左手尺侧感觉较右手减退,右上肢感觉及活动正常。下肢感觉及肌力正常,巴宾斯基征阳性。术前全脊柱X线片及三维CT重建示颈胸段后凸畸形,C5~T1多节段椎体形成障碍,部分椎体分节不良。全脊柱MRI检查无脊髓空洞、脊髓纵裂、脊髓拴系等髓内异常表现。入院诊断:(1)先天性颈胸段侧后凸畸形伴不全瘫;(2)Horner综合征;(3)臂丛神经损害。患者入院后予Halo-重力牵引,3个月后行脊柱后路矫形内固定植骨融合手术,术后予以Halo-vest支具制动半年。伴发的Horner综合征及臂丛神经损害予以保守治疗。术后8个月随访,患者眼睑下垂较术前好转。术后3.4年随访,患者仍残留有左侧眼睑下垂,但较术前明显好转(图2)。随访过程中患者臂丛神经损害症状较术前无明显改善。

讨论
头颈部交感神经传导通路包括三级神经元,即中枢、节前和节后神经元。位于下丘脑的中枢神经元发出交感神经纤维,经脑干、脊髓下行至位于C8~T3脊髓灰质侧角的节前神经元,由此发出的节前纤维随相应脊神经前根出椎间孔后经白交通支进入椎旁的星状神经节,穿过星状神经节后,节前纤维在颈交感干内上行至颈上神经节换元,由节后神经元发出节后纤维沿颈动静脉表面走行,进入头面部和颈部的靶器官如瞳孔开大肌、上睑提肌、头颈部汗腺及平滑肌等。该传导通路的任何一处损伤均可引起Horner综合征。与成人不同的是,儿童Horner综合征多为节前纤维受损所引起,且儿童Horner综合征的表现常不典型,并不一定同时出现瞳孔缩小、眼睑下垂、患侧面部无汗等症状。Root等曾报道1例无明显外伤史的学龄前儿童因颈胸段自发性硬膜外血肿而发生Horner综合征,仅表现为一侧瞳孔缩小伴眼睑下垂。Mutalib等报道1例因气胸压迫胸膜顶的交感神经纤维而导致Horner综合征的儿童,初期仅表现为头痛和广泛的眼球红染。在解剖学上颈胸交界区特指C7~T1段,而临床上则常将位于C6~T4这一区域内无论是否分节的半椎体均称为颈胸段半椎体。颈交感神经通路中位于C8~T3脊髓灰质侧角的节前神经元以及相应节段椎旁的星状神经节均位于颈胸交界区,这是颈胸段半椎体造成颈部交感神经压迫受损的解剖学基础。我们收治的2例颈胸段半椎体畸形患者,顶椎均位于C7~T2区域内的节前神经元及星状神经节位置。
根据患儿临床表现,我们推测2例患儿因为椎体发育异常引起主弯凹侧压力集中,从而压迫了颈交感神经,造成同侧Horner综合征的发生。但由于回顾性研究的局限性,我们缺乏颈交感神经受压的确切影像学资料。颈胸段的C8和T1神经根构成了下臂丛神经,因此颈胸段半椎体在引起Horner综合征的同时也可能造成臂丛神经的损害。我们收治的病例2伴有明显的臂丛神经损害症状,影像学检查示该患者C6、C7、T1椎体左侧形成障碍。笔者认为,该患者的颈胸段半椎体使得头颈部压力集中压迫在凹侧顶椎区域,C7、T1椎体间出现半脱位,对该部位的颈交感神经节造成压迫的同时也压迫了臂丛神经,造成臂丛神经损害。对于颈胸段半椎体伴神经功能损害的患者,我们认为早期手术是有必要的。早期手术治疗可对局部脊柱起支撑作用,缓解凹侧压力,对于引起侧凸或后凸的责任半椎体予以切除可直接解除神经压迫。我们收治的2例患者在术后随访过程中,眼睑下垂均得到了一定程度的改善也证实了这一点。
需要注意的是,颈胸段半椎体畸形患者常合并椎旁神经和血管的发育畸形,手术置钉及截骨等操作对椎旁神经、血管造成损伤的风险极大,因此也需警惕医源性Horner综合征的发生。Deburge等曾报道了1例行前后路联合C7半椎体切除手术的颈胸段半椎体患者术后出现一过性的Horner综合征。Chen等也曾报道在行单一后路半椎体切除手术的18例颈胸段半椎体患者中,1例患者术后出现Horner综合征,但予以保守观察治疗3个月后患者症状缓解。
另外,目前普遍认为Horner综合征的治疗应主要针对原发疾患,该征本身一般仅需对症支持治疗。Kim等指出因上胸椎后纵韧带骨化导致Horner综合征的患者在行后路椎板切除减压术后患者瞳孔不等大及一侧脸部无汗的症状可以得到改善。文献中报道T1、T2节段椎间盘突出压迫引起的Horner综合征患者在行局部减压手术或者保守治疗后患者Horner综合征相关症状均可得到一定程度改善。而对于颈胸段半椎体引发的Horner综合征的患者,我们认为通过切除责任半椎体及内固定手术稳定脊柱对于预防神经功能损伤加重及促进神经功能恢复具有重要意义。
原始出处:
李洋,朱泽章,史本龙,刘臻,孙旭,王斌,邱勇.颈胸段半椎体畸形伴Horner综合征2例报道[J].中国脊柱脊髓杂志,2019,29(07):669-672.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#颈胸段#
37
#畸形#
29
#椎体#
42
#综合征#
39