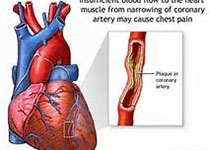
JACC:NOACs相比华法林对房颤患者肾脏影响更小
2017-11-22 MedSci MedSci原创
终身口服抗凝药,比如华法林和非维生素K拮抗剂口服抗凝药(NOAC),被推荐用来预防房颤患者卒中的发生,最新的研究认为在肾功能影响方面NOACs可能比华法林更佳。本研究的目的旨在比较评估四种口服抗凝药(阿哌沙班、达比加群、利伐沙班和华法林)对四种肾脏预后结局的影响:肾小球滤过率(eGFR)下降≥30%、血清肌酐水平加倍、急性肾损伤(AKI)和肾衰。本研究纳入了2010年十月至2016年四月开始口服抗
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JACC#
43
#ACS#
39
#ACC#
39
#NOAC#
46
#NOACs#
40
#房颤患者#
0
学习了不少事情!!
58