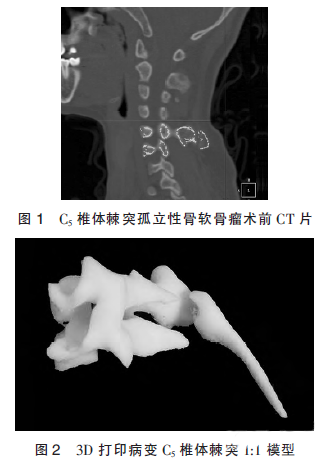
Advanced Materials Technologies:超逼真器官!3D打印更上一层楼
2017-12-11 佚名 中国生物技术网
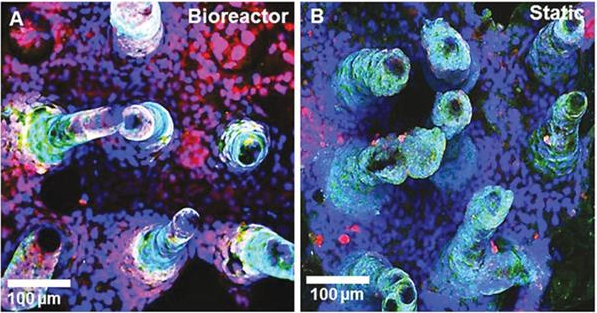
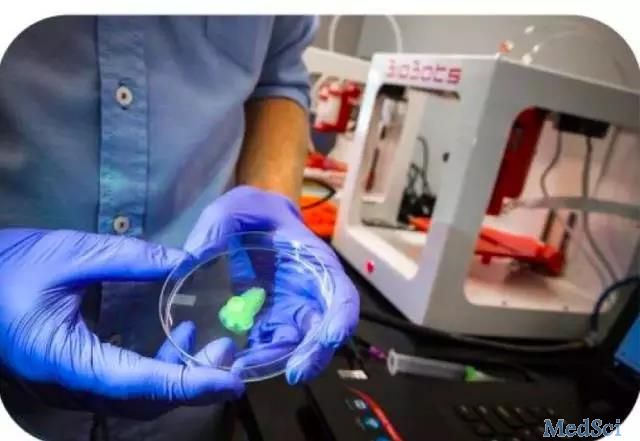
现如今,3D打印已经风靡全球,医疗领域从此项技术中获益尤其多。到目前为止,研究人员使用该技术已打印出了人类软骨、皮肤,甚至是假肢,而我们对于3D打印潜在能力的理解才刚刚开始。现在,明尼苏达大学的研究人员已经开发出了令人难以置信超级逼真的人造器官模型。这项研究成果刚刚发表在《Advanced Materials Technologies》期刊上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#TEC#
24
#Advanced#
31
#3D#
24
谢谢分享学习了
43