新研究发现,ACEI 和 ARB 降低糖尿病肾病患者终末期肾病的发病率
2022-08-30 MedSci原创 MedSci原创 发表于上海
ACEI 和 ARB 药物对糖尿病肾病患者的肾脏具有保护作用,但是仍需要更多的RCT研究,观察不同剂量和用药方案的有效性和安全性。
近年来,我国糖尿病发病率逐渐上升,据数据显示,我国约有1.3亿糖尿病患者。众所周知,糖尿病最可怕的不是高血糖,而是伴随高血糖而来的各种并发症。其中,糖尿病肾病是糖尿病最常见的并发症之一。然而,糖尿病肾病引起的终末期肾病(ESRD)的比例越来越高。
血管紧张素转化酶抑制剂(ACEI)和血管紧张素 II 受体阻滞剂(ARB)具有明确降压作用,尤其适用于伴有心力衰竭、心肌梗死后、糖尿病、慢性肾脏疾病的患者,有充足证据证明可改善预后。ACEI 和 ARB用于蛋白尿患者,可降低尿蛋白,具有肾脏保护作用,但双侧肾动脉狭窄、肌酐(Cr) ≥3mg/dl(265µmol/L)的严重肾功能不全及高血钾的患者禁用。
有研究显示,与其他降压药相比,ACEI和ARB在治疗糖尿病肾病方面效果更好。然而,有些研究显示,虽然 ACEI 可以抑制血清肌酐的升高,但并不影响 ESRD 的发生率。因此,需要更多的研究对ACEI和ARB药物是否能降低糖尿病肾病患者的ESRD发病率进行探讨。
近日,在Comput Math Methods Med杂志发表了一项荟萃分析,旨在探讨ACEI或ARB对糖尿病肾病患者ESRD发病率的影响。
ACEI和ARB 类药物这个种类繁多,其中ACEI常用药有卡托普利、依那普利、赖诺普利及雷米普利等,而ARB常以「沙坦」命名,包括缬沙坦、氯沙坦、厄贝沙坦、替米沙坦、坎地沙坦、奥美沙坦和阿利沙坦。
其中,厄贝沙坦降压幅度较大,单药控制血压的达标率较高,吸收度高,药效持续时间长,在治疗高血压中占有重要地位。
研究人员对 PubMed、Embase、Medline、CENTRAL 和 CNKI 数据库进行文献检索,共检索到2486篇文献,根据文献筛选标准,最终纳入文献11篇,包含7595名糖尿病肾病患者,其中ACEI/ARB药物干预组3793 名患者中有 337 名患者发展成 ESRD,安慰剂对照组3802名患者中有 423 名 患者发展成ESRD。综合分析显示,与安慰剂相比,接受ACEI/ARB药物治疗的 ESRD 患者的 RR 为 0.79。
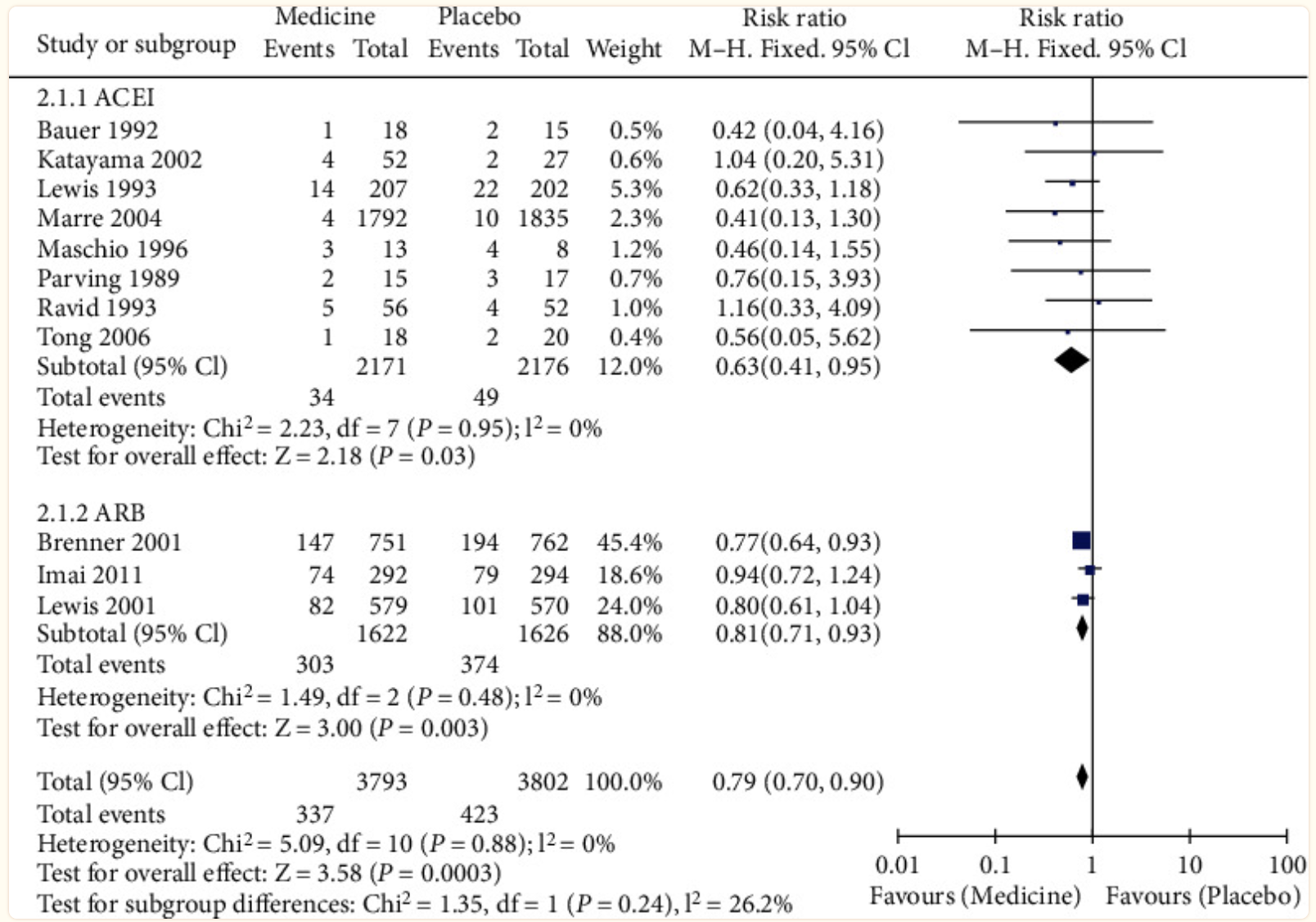
图:ACEI 和 ARB 对终末期肾病发病率的影响.
根据不同药物进行亚组分析,分为ACEI和ARB亚组。8 篇文献被纳入 ACEI 亚组。与安慰剂相比,ACEI干预后,ESRD患者的RR 为0.63。三篇文章被纳入 ARB 亚组,与安慰剂相比,ARB干预后,ESRD患者的RR 为0.81。
综上,ACEI 和 ARB 药物对糖尿病肾病患者的肾脏具有保护作用,但是仍需要更多的RCT研究,观察不同剂量和用药方案的有效性和安全性。
原始出处
Deng X, Li D, Tang Q, Chen Y. ACEI and ARB Lower the Incidence of End-Stage Renal Disease among Patients with Diabetic Nephropathy: A Meta-analysis. Comput Math Methods Med. 2022 May 31;2022:6962654. doi: 10.1155/2022/6962654. PMID: 35685896; PMCID: PMC9173958.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#ACE#
58
#发病率#
64
#终末期#
52
#研究发现#
65
#肾病患者#
45
签到学习
32
#终末期肾病#
39