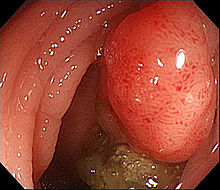
Oncotarget:Beclin 1和LC3可作为预测转移性结直肠癌的生物标志物
2017-09-25 MedSci MedSci原创
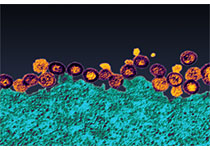
自噬是一种高度保守的代谢过程,表现为细胞对不正常的或不需要的细胞成分的“自食”。自噬在癌症转移中扮演著着重要的角色,而转移性疾病是结直肠癌导致相关死亡的主要原因。
自噬是一种高度保守的代谢过程,表现为细胞对不正常的或不需要的细胞成分的“自食”。自噬在癌症转移中扮演著着重要的角色,而转移性疾病是结直肠癌导致相关死亡的主要原因。研究者在结直肠癌手术标本中研究了免疫组化表达自噬相关蛋白Beclin 1和微管相关蛋白1A/1B-轻链3(LC3)。首先在一个包含205例患者的训练队列中得到初步结果,然后在内部验证队列(160例)和独立的队列(161例)中验证结果。相比非转移性CRC,转移性CRC标本中Beclin 1和LC3的表达较低。此外,我们开发了一种基于自噬的转移预测分类器。在训练队列中,这种分类器通过检测包括Beclin 1、LC3和CEA水平在内的生物指标,预测结直肠癌转移的敏感性达到了82.9%,特异性达到89.8%。在独立队列中,预测结直肠癌转移的敏感性为77.9%,特异性为90.3%。这些结果表明,LC3和Beclin 1低表达与更具侵略性的癌细胞表型有关。并且,本研究中的自噬分类器是预测CRC转移的可靠工具。原始出处:Hong Zhao,Maopeng Yang,Bin Zhao,et al.Beclin 1 and LC3 as pre
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#target#
36
#标志物#
28
#转移性#
32
#结直肠#
22
#生物标志#
34
#生物标志#
21