International Journal of Nursing Studies:护士主导的家庭干预能够改善ICU患者家庭结局
2021-10-06 小文子 MedSci原创
多学科护士主导的家庭干预能够改善患者家庭结局。
进入ICU治疗的患者通常会给患者及其家人带来情绪和经济上的痛苦,引起焦虑、抑郁、悲伤和创伤后应激障碍等,从而影响患者及其家人的健康状态。同时,COVID-19的大流行加剧患者进入ICU的后果,导致家庭面临更多的心理社会问题。因此,护士和医生需要及时了解支持危重患者家属的干预措施。
发表在护理权威杂志International Journal of Nursing Studies的一篇文章系统评价护士主导的家庭干预改善成人ICU家庭结局的证据。并提出以下问题:成人ICU中使用了哪些类型的护士主导家庭干预?护士主导家庭干预措施是否能改善成人ICU的家庭结局?
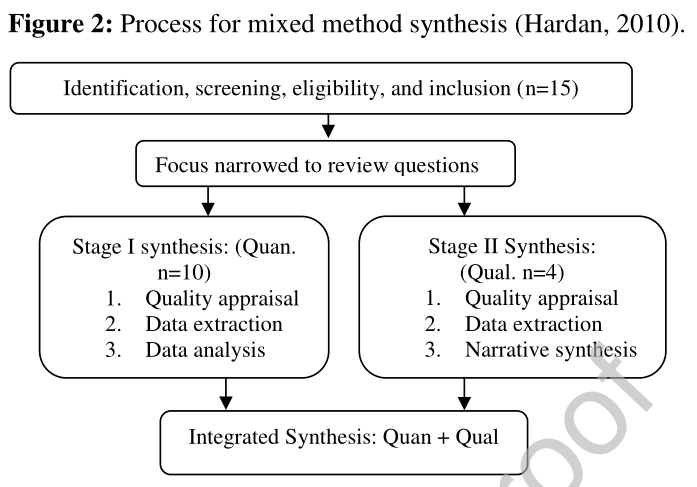
研究人员检索2010年1月至2020年10月期间相关的研究。最终纳入15项研究,干预措施分为五类:教育/信息,家庭参与护理,日记,以及集束化干预策略。这些分类在包含要素、干预方式和家庭结局各不相同。其中,11项研究显示护士主导干预措施能够改善家庭结局。具体而言,教育/信息干预改善家庭支持,增强家庭对护理的满意度;日记可以促进家庭成员对疾病严重程度的理解,促进家庭成员的心理健康;集束化干预措施能够节约成本、提高沟通质量和以患者为中心的护理。然而,一项研究显示干预后患者情况恶化,两项研究显示这种方法对家庭结局无明显影响。
研究结果表明,干预要素、工具和结果差异反映了家庭需求多样性,并且已经制定多种干预措施促进ICU的家庭健康。证据表明,多学科护士主导的家庭干预能够改善患者家庭结局。
原文出处:
Frank KIWANUKA, BNurs, Natalia SAK-DANKOSKY, et al, The evidence base of nurse-led family interventions for improving family outcomes in adult critical care settings: a mixed method systematic review, International Journal of Nursing Studies (2021), doi: https://doi.org/10.1016/j.ijnurstu.2021.104100
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














不错
38
#studies#
38
#Nat#
0
#eRNA#
35
#DIE#
48
#ICU患者#
42