medRxiv:新冠第四针或非必要,中山大学肖海鹏团队研究证实疫苗保护效果在第三针后饱和
2022-02-28 nagashi “生物世界”公众号
第四剂新冠疫苗是否必要?能否应对奥密克戎?肖海鹏团队证明反复接种新冠疫苗将导致疫苗效用降低,并造成免疫应答向非RBD结构域转移!
第四剂新冠疫苗是否必要?能否应对奥密克戎?肖海鹏团队证明反复接种新冠疫苗将导致疫苗效用降低,并造成免疫应答向非RBD结构域转移!
最近,国内的新冠疫情形势再度紧张了起来,至2月25日,10天内我国本土共新增新冠病例689例,涉及江苏、辽宁、内蒙古、广东等13个省市和自治区。这些新增病例均为德尔塔(Delta)和奥密克戎(Omicron)变异株所致。
根据美国疾病控制与预防中心发病率和死亡率周报(MMWR)的报告,第三剂新冠mRNA疫苗的有效性在奥密克戎(Omicron)为主的时期迅速减弱。为了应对快速衰退的免疫反应和奥密克戎等新冠变异株对一线医护人员的巨大威胁,中山大学附属第一医院肖海鹏教授团队开展了四剂灭活SARS-CoV-2疫苗的初步临床试验。
该研究于近日在预印本平台 medRxiv 上线,论文题为:Four doses of the inactivated SARS-CoV-2 vaccine redistribute humoral immune responses away from the Receptor Binding Domain
研究数据显示,接种第四剂量灭活新冠疫苗是安全的,并且能够在第三剂量6个月后恢复衰退的免疫反应,但第4剂疫苗诱导的RBD-NAbs峰值低于第3次剂量。这表明,反复接种疫苗引发的免疫应答不会一直提高,并且会造成免疫应答向非RBD结构域转移的情况。
研究团队表示,免疫应答不会随着接种次数的增加而不断提高,因此反复接种疫苗不是应对奥密克戎(Omicron)及将来可能出现的其他变异株的有效策略。开发一种具有更多不同抗原表位、能够诱导中和抗体对抗变异株的新型疫苗才是未来新冠疫苗“加强针”的发展方向。

疫苗是预防COVID-19等传染病的最具成本效益的方法之一。在持续了两年多时间的COVID-19大流行中,数十亿剂新冠疫苗已在世界各地分发,在对抗SARS-CoV-2感染和相关住院方面取得了良好的效果。
然而,接种两剂新冠疫苗后,疫苗诱导的免疫反应会在6个月内迅速减弱。因此,不少国家也推出了接种新冠疫苗“加强针”的策略。但随着德尔塔、奥密克戎等新冠变异株的相继出现,基于原始病毒株开发的疫苗接种系统也受到了巨大挑战,由此提出了一个新的疑问——仅仅依靠接种“加强针”就足以预防新冠变异株吗?
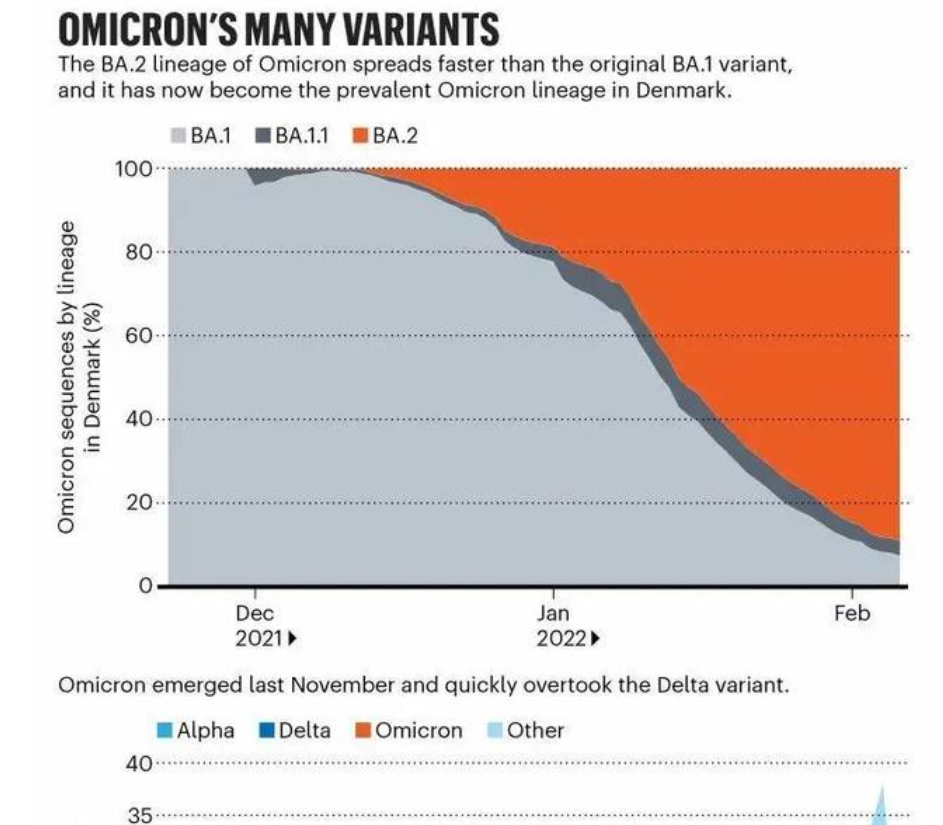
奥密克戎成为主要流行病毒株
就以奥密克戎为例,该突变株携带超过30种突变,这些突变使其具有强大的免疫逃逸能力,世界范围内也报告了许多奥密克戎突破性感染病例。虽然接种第三剂疫苗可以在一定程度上预防奥密克戎,但“加强针”提供的保护并不是完全的,而且还在快速减弱。
美国疾病控制与预防中心最近的一份报告显示,在接受3剂mRNA疫苗的人群中,对急诊科和急诊护理人员的保护率在4个月内从87%下降到66%,在奥密克戎占主导的时期,5个月后进一步下降到31%。因此,以色列在一月份开始向包括医护人员在内的最脆弱人群提供第四剂疫苗。
在这项研究中,肖海鹏团队对由38名医护人员组成的研究队列进行监测。研究人员首先观察了该队列对第三剂新冠灭活疫苗诱导的免疫应答,考虑到在接种第三剂6个月后只有15%参与者的体液免疫反应仍然存在,38名医护人员自愿接种第四剂量灭活疫苗。
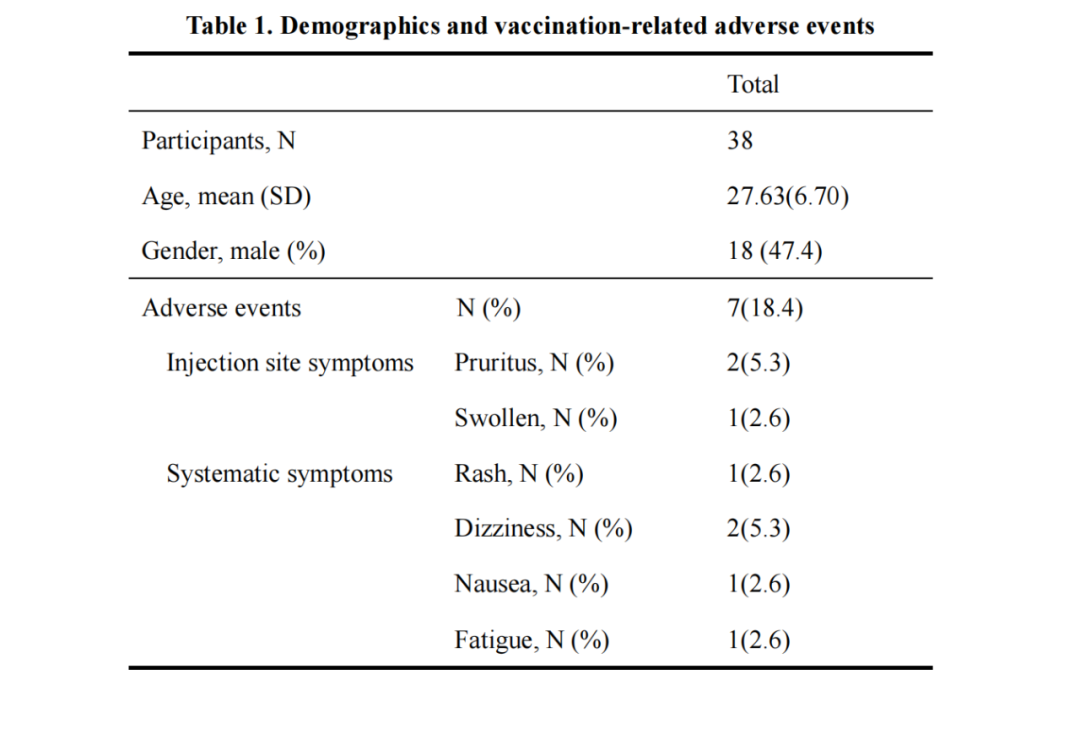
由38名医护人员组成的研究队列
研究证明接种第四剂灭活疫苗是安全的,并且能够在接种第三剂疫苗6个月后重新唤醒衰退的免疫反应。然而,在第三次注射后,受试者的免疫反应更强,但整体中和抗体(NAbs)和针对新冠病毒刺突蛋白(S蛋白)受体结合域(RBD)的NAbs的诱导受到更大的抑制。
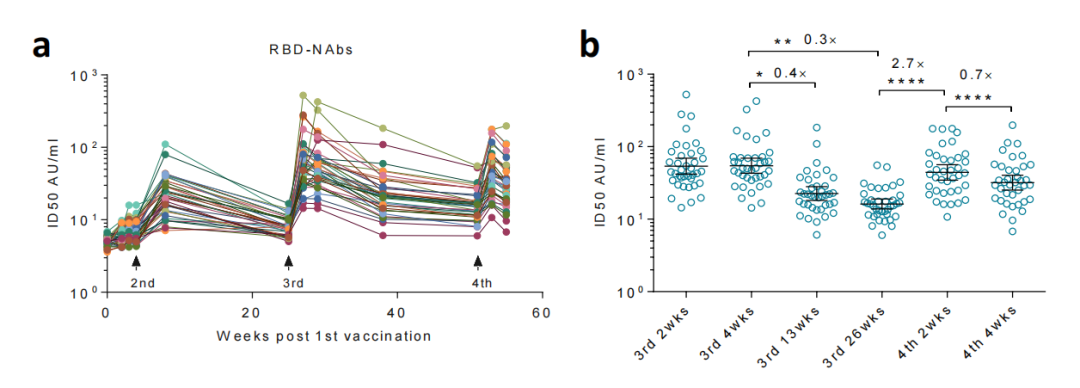
第3剂量引起的有效免疫反应抑制了第4剂量后RBD-NAbs的诱导
令人意外的是,从第1次接种到第3次接种,疫苗所诱导的RBD-NAbs逐步升高,但在第4次接种后来到了一个“转折点”——第4次剂量诱导的RBD-NAbs峰值低于第3次剂量诱导的RBD-NAbs峰值。
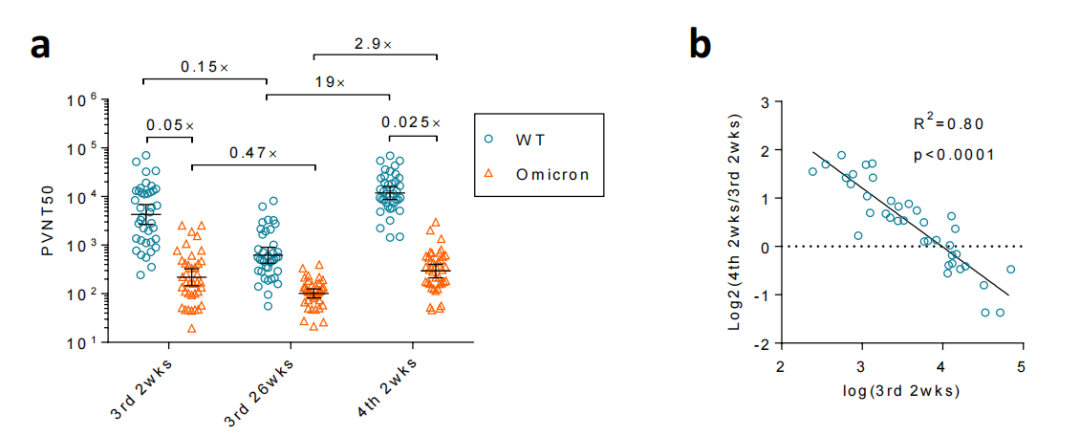
第四剂新冠灭活疫苗增强了抗原始病毒株的NAbs,但对奥密克戎无效
并且,伴随着RBD-NAbs诱导的减少,免疫系统对新冠病毒的核衣壳蛋白(NP)以及刺突蛋白的N端结构域(NTD)的免疫反应增强。尽管针对NTD的抗体也能够中和奥密克戎突变株,但由于Omicron-NTD发生了重大构象变化,因而第四剂疫苗对奥密克戎突变株的整体效用降低了不少。
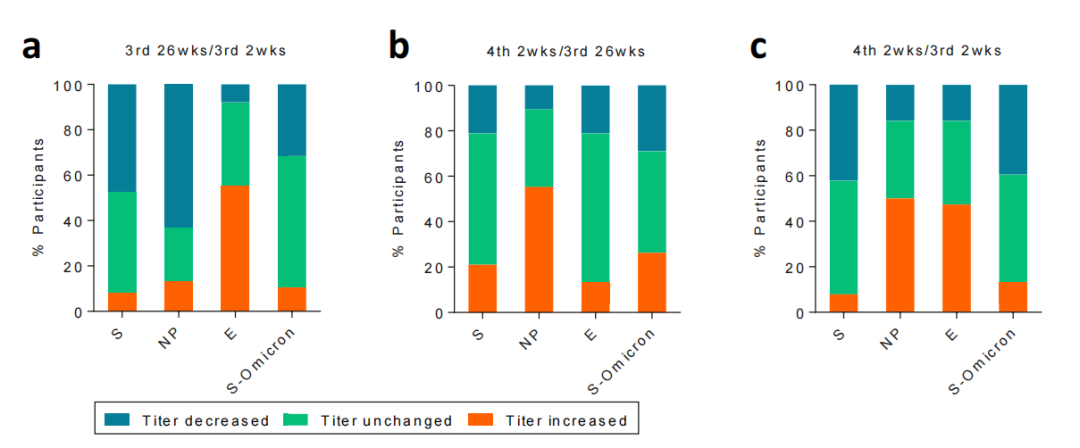
体液免疫反应由S蛋白转向NP蛋白
总而言之,这项纵向临床研究监测了同一人群对每一剂疫苗的免疫反应,以此建立疫苗对突变株病毒的中和效力的动态关系。研究结果表明,免疫应答不会随着接种次数的增加而不断提高,而且在反复接种疫苗后,会出现集中于一个亚基的免疫应答被抑制,同时免疫应答向其他亚基转移的情况。
因此,研究团队表示,为了应对不断进化的新冠病毒变异株,一种具有更多不同抗原表位、能够诱导NAbs对抗突变株的新型疫苗将是未来新冠疫苗“加强针”的发展方向。
此外,以色列的研究人员也于近日在预印本平台 medRxiv 发表文章,显示第四剂mRNA接种会提高中和抗体水平,但对新冠病毒感染的防护作用几乎没有帮助。这也说明了大多数人可能并不需要接种第四针新冠疫苗。

以色列研究团队认为,对于那些年轻健康且没有感染风险因素的人来说,可能不会从第四剂接种中受益多少,但第四剂可能对重病风险较高的人有益,目前,以色列、智利和瑞典等国家正在向老年人和其他高风险群体提供第四剂疫苗接种。
原始出处:
Ji Wang, Caiguangxi Deng, Ming Liu, et al. Four doses of the inactivated SARS-CoV-2 vaccine redistribute humoral immune responses away from the Receptor Binding Domain. medRxiv, 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#medRxiv#
41
#中山大学#
48
#Med#
31
学到了很多东西,谢谢各位老师的指导
58
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
55
学习
55
学习了
49