Mov Disord : 新型左旋多巴肠道凝胶,可有效减缓帕金森的运动障碍表现
2021-09-25 Freeman MedSci原创
左旋多巴-卡比多巴的组合是帕金森病(PD)治疗的主流。一般来说,儿茶酚-O-甲基转移酶(COM-T)抑制剂、单胺氧化酶-B(MAO-B)抑制剂和多巴胺激动剂与左旋多巴同时使用以减少运动波动。尽管使用了
左旋多巴-卡比多巴的组合是帕金森病(PD)治疗的主流。一般来说,儿茶酚-O-甲基转移酶(COM-T)抑制剂、单胺氧化酶-B(MAO-B)抑制剂和多巴胺激动剂与左旋多巴同时使用以减少运动波动。尽管使用了最佳的口服药物,患者还是会逐渐出现持续的运动波动,如消退和延迟的 "开启 "时间,其特点是可预测或不可预测的从移动到不移动的摆动。即使采用最佳的口服治疗方法,运动障碍的处理也往往具有挑战性。
运动障碍是晚期PD最麻烦的症状之一。大约50%的患者在开始治疗后4-5年出现运动障碍,大约90%的患者在9年后出现运动障碍。中度至重度运动障碍可引起疼痛并损害自主运动,从而影响生活质量(QoL)。运动障碍被认为是由多次口服左旋多巴引起的突触后多巴胺能受体的脉冲性刺激造成的。
在严重的神经变性、不稳定的吸收、不可预测的胃排空变化和短的左旋多巴半衰期的背景下,多次口服左旋多巴可以导致血浆中左旋多巴水平的不稳定,因此,基底神经节中的多巴胺水平也不稳定。
因此,PD的运动障碍可能来自于药物治疗,特别是左旋多巴治疗。运动障碍的治疗方案包括口服金刚烷胺、持续皮下输注阿扑吗啡和脑深部刺激(DBS)。然而,DBS不一定适用于所有患者。晚期PD患者需要更多的治疗选择。一种选择可能是持续的左旋多巴输送。
左旋多巴-卡比多巴肠道凝胶(LCIG)是通过经皮内窥镜胃造口术与J管延伸(PEG-J)使用外部泵持续输送到上肠。与标准的口服左旋多巴治疗相比,LCIG提供了更稳定的左旋多巴血浆水平,从而减少了运动并发症和运动障碍的可能性。LCIG的临床试验和观察研究表明,"关闭 "时间明显减少,"开启 "时间减少并伴有运动障碍,"开启 "时间增加而无运动障碍的困扰。
然而,这些研究使用患者PD日记和/或帕金森病统一评定量表(UPDRS)的运动部分(第四部分)来评估运动障碍,这两种方法对变化的敏感性和量化运动障碍症状的能力都很有限。
统一运动障碍评定量表(UDysRS)的开发是为了评估患者 "开 "运动障碍和 "关 "肌张力障碍的历史性残疾,对运动障碍的严重程度和分布进行客观评价,并提供衡量运动障碍几个方面的度量属性。目前还没有随机的临床试验来比较LCIG对运动障碍的有效性与使用UDysRS的优化医疗(OMT)。
藉此,西班牙University General Hospital of Elche,的Eric Freire-Alvarez等人在晚期帕金森病患者中进行了一项为期12周的随机研究,通过UDysRS和帕金森病日记来评估LCIG与OMT在运动障碍症状方面的有效性。
此外,他们还比较了LCIG与OMT在运动波动、健康相关结果、安全性和耐受性方面的差异。
在这项3b期、开放标签、多中心、为期12周的干预性研究(NCT02799381)将63名未接受LCIG治疗的晚期PD患者(UDysRS≥30)随机分配到LCIG(N = 30)或OMT(N = 33)治疗。运动障碍的影响在基线至第12周使用UDysRS进行评估。还评估了与PD相关的运动和非运动症状,以及生活质量(QoL)。
12周后,与OMT组(n = 26;-2.33 ± 2.56)相比,LCIG组(n = 24;-17.37 ± 2.79)UDysRS测量的运动障碍明显减少(-15.05 ± 3.20;95% CI,-21.47至-8.63;P < 0.0001)。
在第12周,LCIG与OMT相比,在没有麻烦的运动障碍的 "在位 "时间(P = 0.0001)、QoL(P < 0.0001)、全局变化印象(P < 0.0001)、日常生活活动(P = 0.0006)和统一帕金森病评分表(UPDRS)第三部分(P = 0.0762)方面也有明显改善。
27名(44.3%)患者报告了治疗中出现的不良事件(LCIG,18[64.3%];OMT,9[27.3%])。2名(7.1%)接受LCIG治疗的患者发生了严重不良事件。
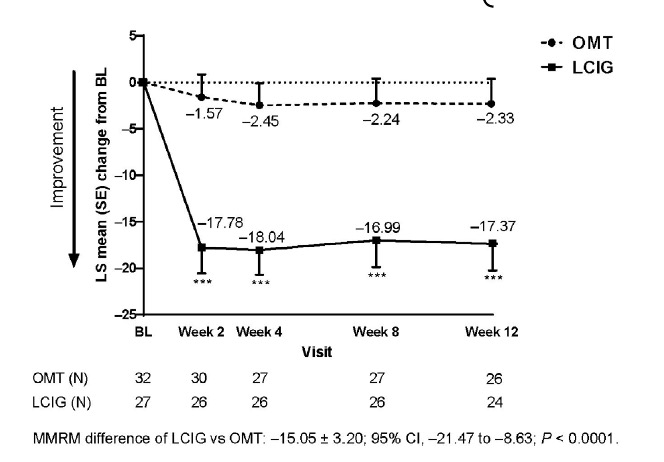 与OMT相比,LCIG明显减少了运动障碍的发生。LCIG在治疗晚期PD患者麻烦的运动障碍方面显示出疗效,同时在运动和非运动症状以及QoL方面都显示出益处。
与OMT相比,LCIG明显减少了运动障碍的发生。LCIG在治疗晚期PD患者麻烦的运动障碍方面显示出疗效,同时在运动和非运动症状以及QoL方面都显示出益处。
原文出处:
Freire‐Alvarez E, Kurča E, Lopez Manzanares L, et al. Levodopa‐Carbidopa Intestinal Gel Reduces Dyskinesia in Parkinson’s Disease in a Randomized Trial. Mov Disord. Published online July 8, 2021:mds.28703. doi:10.1002/mds.28703
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#Dis#
45
#Disord#
38
#运动障碍#
37
#凝胶#
0
#左旋多巴#
63