第十七届中国介入心脏病学大会(CIT2019)|朱鲜阳:结构性心脏病介入治疗并发症及其防治
2019-03-30 Vina MedSci原创
我国先心病介入治疗发展历程如下图所示。现在,常见先心病60~70%都是通过介入的方法得到解决。我国目前已开展的先心病介入项目如下图所示。先心病介入治疗并发症分类。常见先心病介入治疗并发症。介入器材移位或脱落,很多和操作技术不规范有关!动脉导管未闭病例,封堵器脱落后重新植入。心包积液在房缺最多见。也见于二尖瓣球囊扩张。临床上发现器械移位,一般与超声经验和图像看不清有关。对于器械的辨别,一定要在术中仔
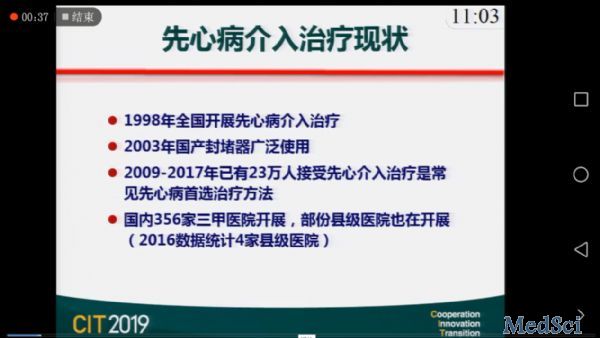
我国先心病介入治疗发展历程如下图所示。现在,常见先心病60~70%都是通过介入的方法得到解决。
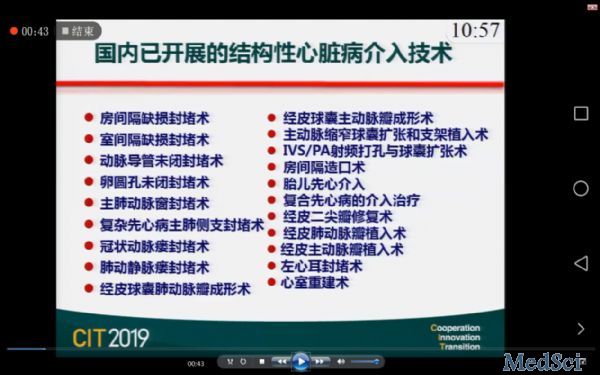
我国目前已开展的先心病介入项目如下图所示。
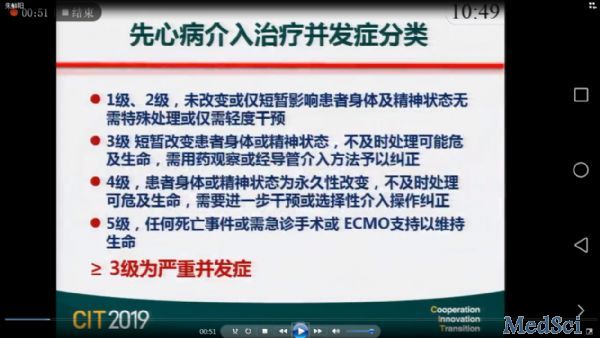
先心病介入治疗并发症分类。
常见先心病介入治疗并发症。
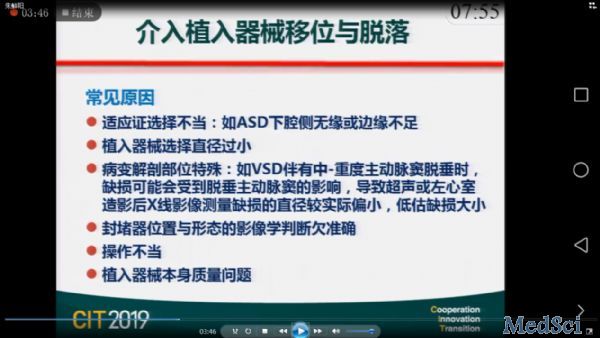
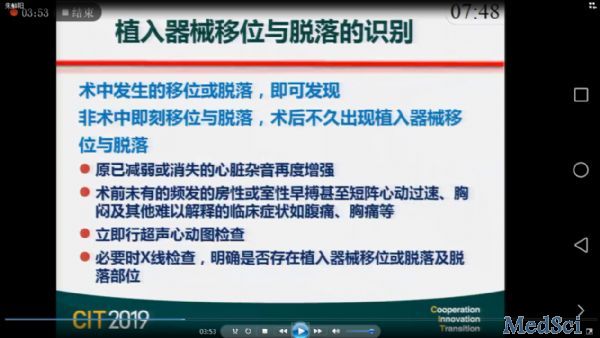
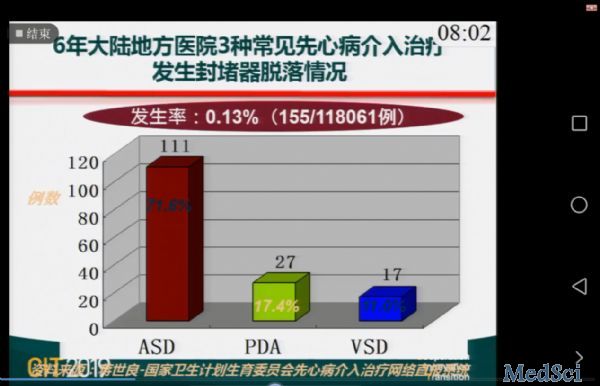
介入器材移位或脱落,很多和操作技术不规范有关!
动脉导管未闭病例,封堵器脱落后重新植入。
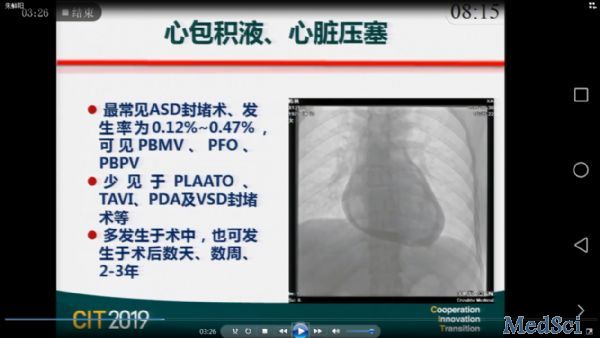
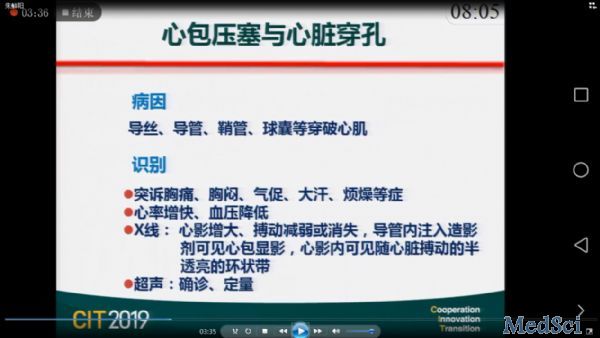
心包积液在房缺最多见。也见于二尖瓣球囊扩张。
病例:做完房缺封堵器后1年,病人出现明显紫绀(嘴、手指)。发现封堵器脱位至下腔静脉开口处,使下腔血直接进入左房,造成紫绀。说明有些较大的封堵器未必会马上脱落,但可能在间隔上移位,引起完全房室传导阻滞。
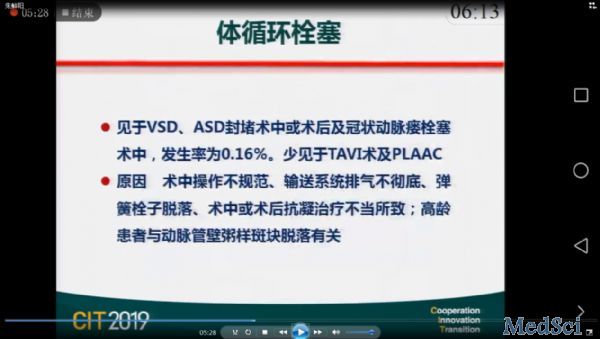
体循环栓塞的发生与操作密切相关,医生应从培训开始就要十分慎重。
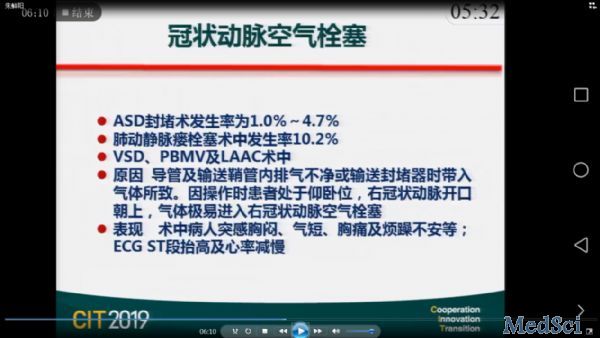
冠脉空气栓塞主要发生在房缺。高压系统不易出现,低压系统容易出现,必须慎重处理。
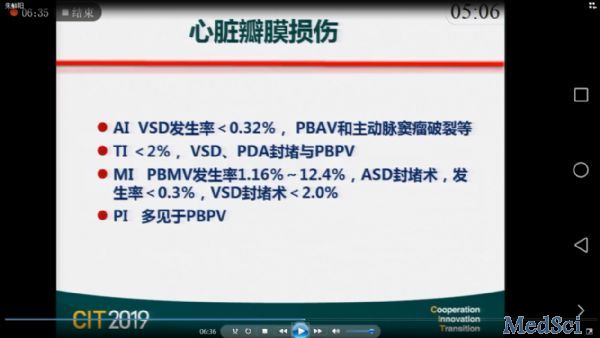
心脏瓣膜损伤。所有经过三尖瓣的动脉导管未关闭及动脉瓣的狭窄,在经过三尖瓣时不要将导丝缠过去。低级错误应该避免!可以通过操作避免。一旦出现,尽快找外科做修复手术,不要耽误时间太长。
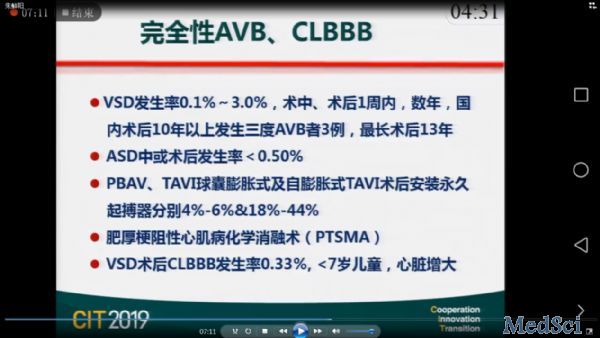
完全房室传导阻滞和完全性左束支阻滞。
我国术后发生AVB最长时间为13年。但根据文献,外科术后即使过了30、40年,病人也还是可以出现完全房室传导阻滞,可能与病人本身传导系统的发育异常有关。
1例罕见病例:患者主动脉窦瘤,无冠窦瘤破入右房,术后3天出现完全房室传导阻滞。全球文献中仅有2例报道。房室窦引起的传导阻滞可能跟它的位置或koch三角比较近,猜测是在选择封堵器时磨到koch三角,引起水肿,导致完全传导阻滞。病人植入临时起搏器3天后恢复,健康出院。
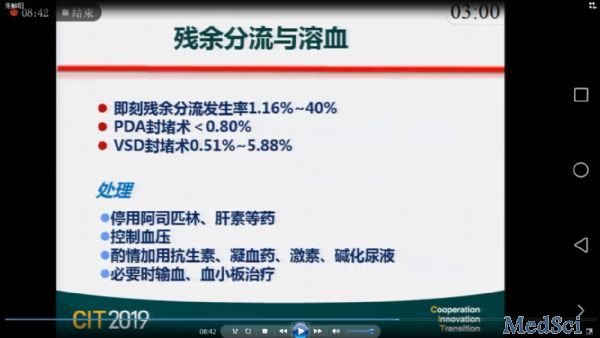
残余分流与溶血。残缺分流在室缺动脉导管内壁最多见,部分可在房缺中见到。这样的病人一般有机械性损伤、血小板减少、肝素诱导的血小板减少。但在先心病中,肝素诱导的血小板减少非常少见。
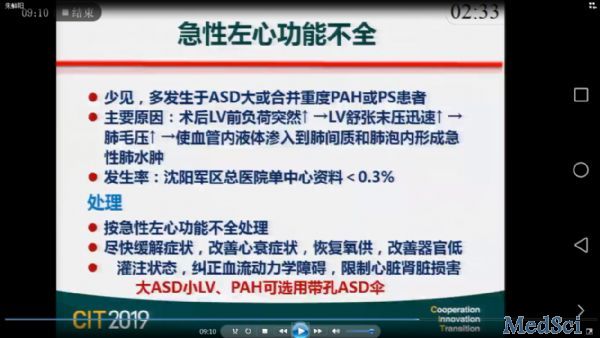
急性左心功能不全。一般出现于大的房缺,尤其是年龄比较大的、左室内径比较小的患者,此时操作要小心。一般来说大的房缺,左室特别小,由于长期右心负荷,压迫左心室。如果病人肺动脉压较高,且左室小,分流量>30%,Qp/Qs是1.5,则植入带孔ASD伞。放入伞后,病人肺动脉压降幅较大(例:80→40),则不用放带孔伞。
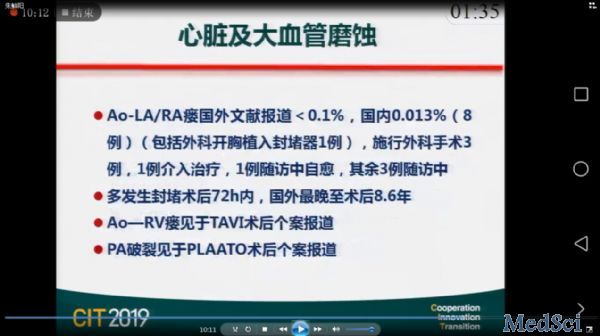
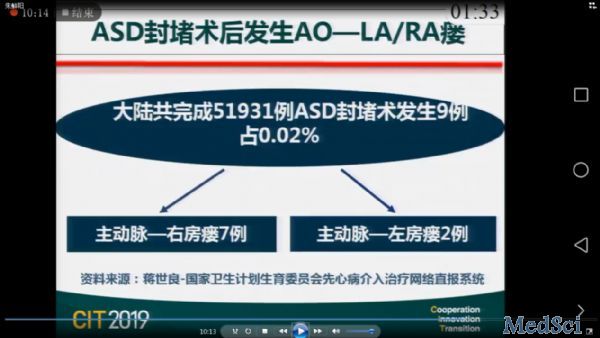
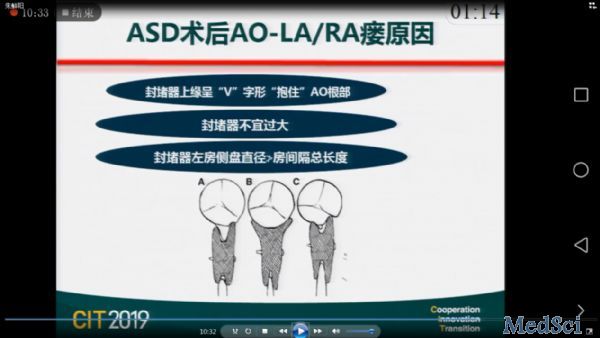
心脏大血管磨蚀。
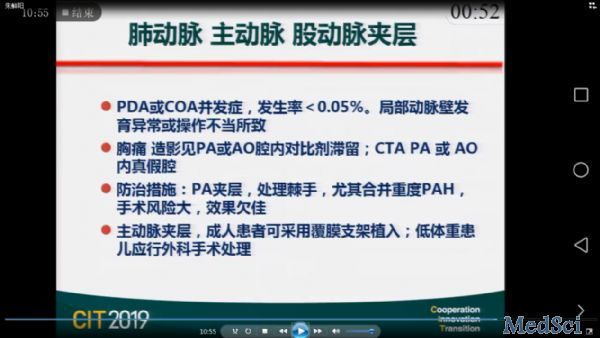
主动脉夹层。室间隔缺损操作过程中到了右冠容易引起夹层。导管操作拽出时也易引起夹层。
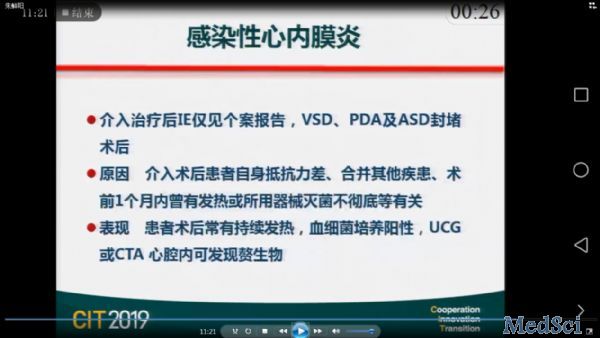
感染性心膜炎。
血管入路并发症。
假性动脉瘤。可以在超声下定点压迫50分钟,加压包扎24小时松绷带,大部分病人可以治愈。实在闭不上可打凝血酶。
股动静脉瘘。
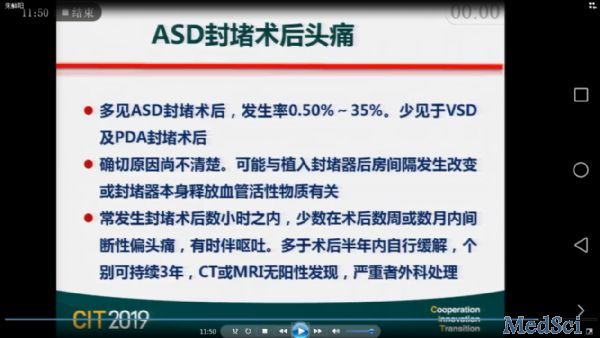
房间隔封堵术后头痛。
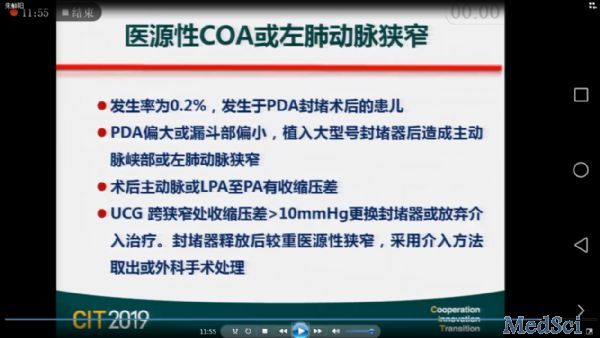
医源性主动脉缩窄或左肺动脉狭窄。
死亡。
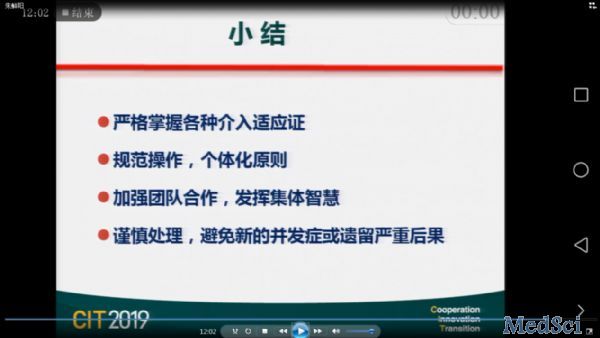
小结:要严格掌握各种介入适应证,不要盲目扩大;规范操作,每个病人都有不同;结构性心脏病团队要发挥合作精神,默契配合;谨慎处理,出现并发症时不要着急,避免出现次生并发症或严重后果。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

























#心脏病学#
27
#结构性#
31
#并发#
31
#介入心脏病学#
42
#CIT#
22