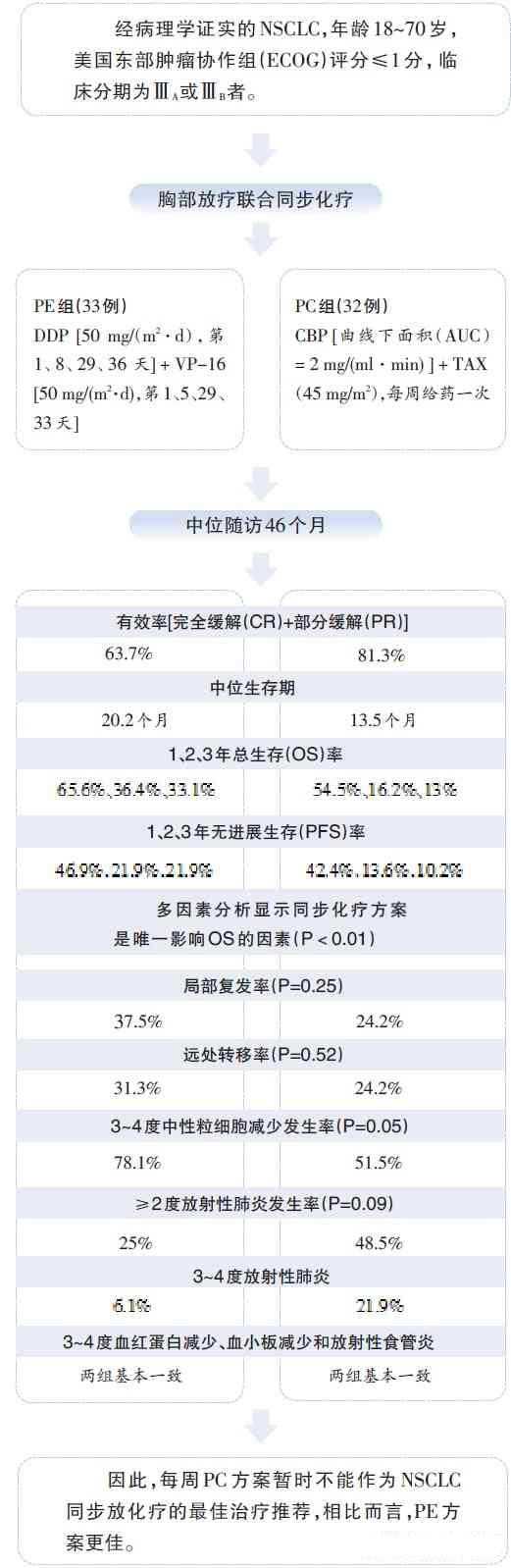
Lung Cancer :局部晚期非小细胞肺癌同步放化疗PE与PC方案比较
2012-08-16 卢秀玲 中国医学论坛报
局部晚期非小细胞肺癌(NSCLC)的标准治疗方案为同步放化疗,虽然目前化疗方案尚不统一,但最常见的两种方案为PE方案[依托泊苷(VP-16)+顺铂(DDP)]和PC方案[紫杉醇(TAX)+卡铂(CBP)]。PE方案较早应用于肺癌同步放化疗中,多项研究均显示PE联合同步放疗较序贯放化疗可延长患者生存期。然而晚期NSCLC的整体预后仍然欠佳。近十年

链接;
Wang L,Wu S,Ou G,Bi N,Li W,Ren H,Cao J,Liang J,Li J,Zhou Z,Lv J,Zhang X.Randomized phase II study of concurrent cisplatin/etoposide or paclitaxel/carboplatin and thoracic radiotherapy in patients with stage III non-small cell lung cancer.Lung Cancer 2012 Mar 12
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PC方案#
42
#局部晚期#
38
#非小细胞#
0
#PE#
36
#放化疗#
35
#局部#
35
#同步放化疗#
24