Neurology:神经反馈技术,有利于脑中风后步态改善
2021-04-30 Freeman MedSci原创
Neurology:神经反馈技术,有利于脑中风后步态改善

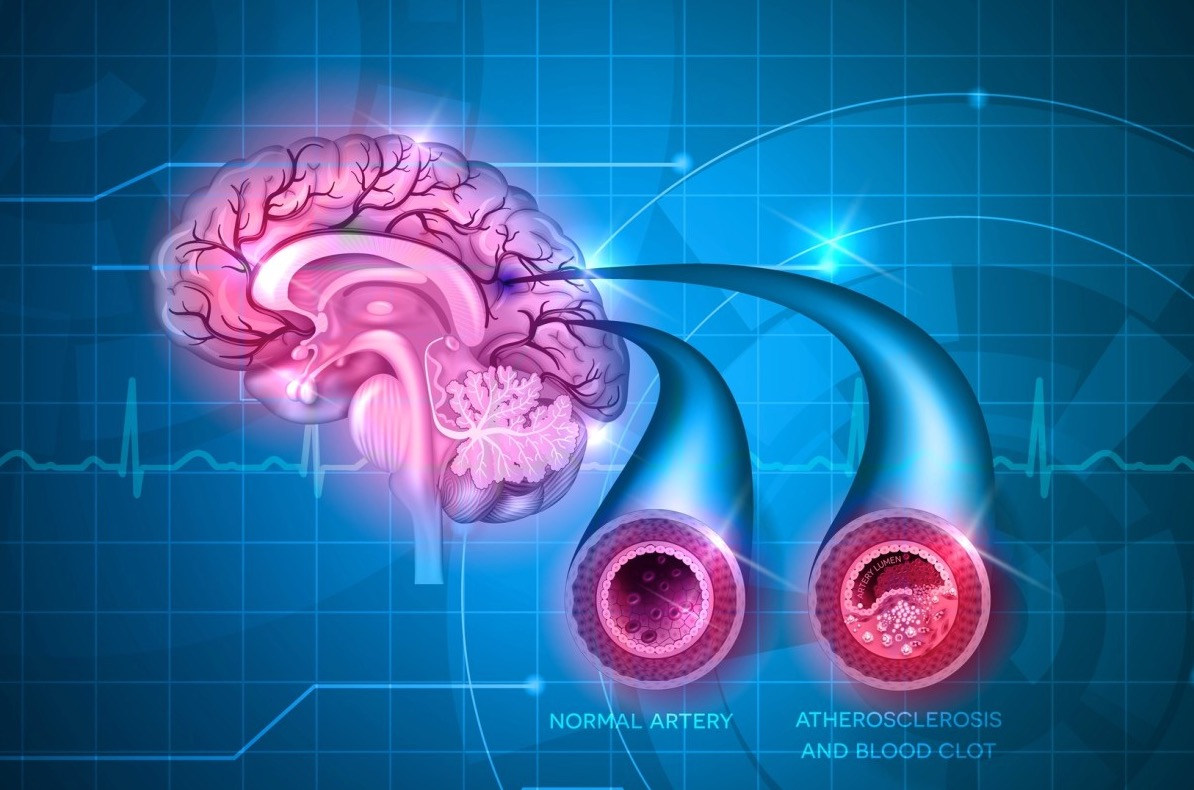
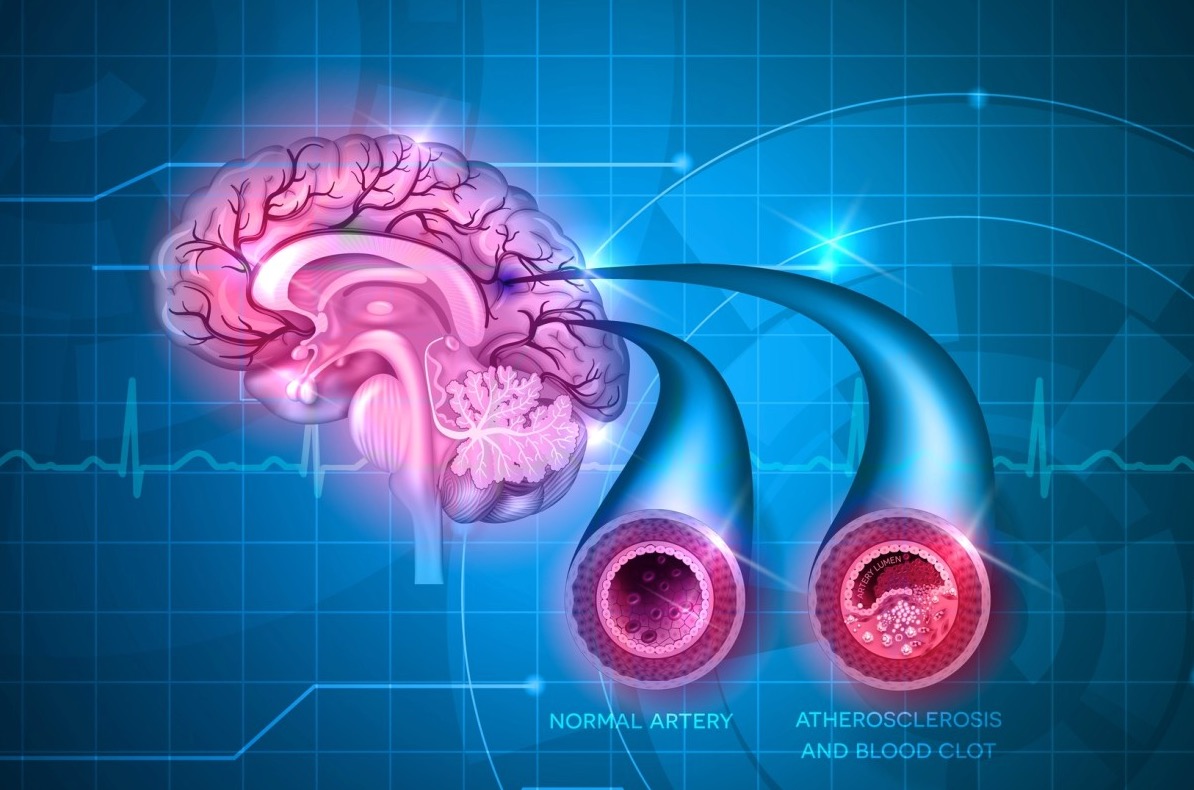
脑卒中后的步态和平衡功能障碍影响了整体生活质量,即使在康复后,20-30%的患者也不能独立行走。研究表明,大多数恢复发生在发病后的头12周内,此后恢复有限。
基于神经网络的实际重组对中风后功能恢复至关重要的研究结果,促进塑性重组的神经调节是一个可行的研究目标。神经反馈是一种神经调节技术,患者通过大脑活动反馈来学习如何调节自己的神经活动。 由于其安全性和便携性,功能性近红外光谱介导的神经反馈(fNIRS-NFB)可能是一种对脑卒中后患者有希望的技术。之前的小型试点研究揭示了fNIRS-NFB对上肢恢复的可行性和疗效。
在神经调控中,目标皮层区域的选择是基于所需的效果,例如外侧运动区用于治疗上肢功能障碍。因此,先验地确定步态和平衡恢复的适当目标尤为重要。在参与步态和姿势调节的各种神经结构中,以前的研究表明。大脑皮层,特别是辅助运动区(SMA)及其下行投射的重要作用。
鉴于对健康的年轻受试者的姿势控制有潜在的有益影响,他们进行了这项双中心、双盲、随机对照试验,以检验假设:用fNIRS-NFB促进SMA会增强由3米步行(TUG)评估的姿势和步态恢复。
藉此,日本大阪大学的Masahito Mihara等人,进行了一项中心、双盲、随机对照试验,纳入54名患者。
他们在皮层下脑卒中引起的轻度至中度步态障碍的患者,在步态和平衡相关的运动想象中,使用fNIRS-NFB进行了6次SMA神经反馈促进治疗。参与者被随机分配到干预组(REAL:28名患者)或安慰剂组(SHAM:26名患者)。在REAL组,fNIRS信号包含参与者的皮质激活信息。主要结果是干预后4周TUG的改善。
他们发现,REAL组比SHAM组,步态改善明显。(5.51±7.64秒,95%CI:2.43-8.60;组间差异7.33秒,95%CI:0.83-13.83;P=0.028)。
只有REAL组的图像相关SMA激活明显增加,SMA和外侧运动前区之间的静止状态连接增强。未发现,与fNIRS介导的神经反馈干预有关的不良反应。
这个研究的重要意义在于:使用fNIRS神经反馈在运动想象中促进SMA,可以通过调节SMA及其相关网络来增强卒中后的步态和平衡恢复。
原文出处:
Effect of Neurofeedback Facilitation on Post-stroke Gait and Balance Recovery: A Randomized Controlled Trial
Masahito Mihara, Hiroaki Fujimoto, Noriaki Hattori, Hironori Otomune, Yuta Kajiyama, Kuni Konaka, Yoshiyuki Watanabe, Yuichi Hiramatsu, Yoshihide Sunada, Ichiro Miyai, Hideki Mochizuki
Neurology Apr 2021, 10.1212/WNL.0000000000011989; DOI: 10.1212/WNL.0000000000011989
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Neurol#
40
#步态#
35
学习
59
学习了
64
厉害
60
中风是俗称,应该称为缺血性卒中吧
52