PNAS:科学家发现先导化合物“饿死”癌细胞
2012-05-28 Beyond 生物谷
近日,一队来自新加坡国立大学(NUS)的生物科学系和机械生物学研究所的科学家团队已经发现一种在研的潜在的药物临床前试验药物的铅化合物可以剥夺癌细胞的能量,阻止肿瘤细胞生长成肿瘤。这种药物的先导化合物被命名为BPTES。 这是第一次有研究能提供证据证实药物的先导化合物能抑制肿瘤的形成。 在新研究发现的基础上,NUS研究团队对这一先导化合物进行了衍生结构修,能更有效地杀死肾脏和乳腺癌细胞。相关研究
近日,一队来自新加坡国立大学(NUS)的生物科学系和机械生物学研究所的科学家团队已经发现一种在研的潜在的药物临床前试验药物的铅化合物可以剥夺癌细胞的能量,阻止肿瘤细胞生长成肿瘤。这种药物的先导化合物被命名为BPTES。
这是第一次有研究能提供证据证实药物的先导化合物能抑制肿瘤的形成。
在新研究发现的基础上,NUS研究团队对这一先导化合物进行了衍生结构修,能更有效地杀死肾脏和乳腺癌细胞。相关研究论文发表在PNAS杂志上。
通过 “饥饿”杀死癌细胞
癌症生物学的经典实验已经证明癌细胞通过谷氨酰胺获得能量。虽然谷氨酰胺是促成这一系列生化反应的第一个酶,但很少有人知道如何控制谷氨酰胺的活性。
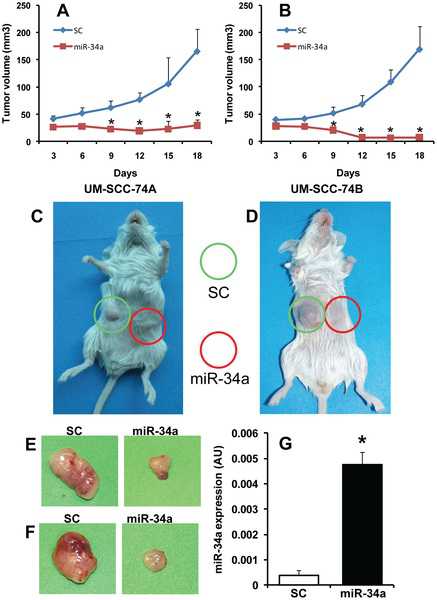
研究小组已经成功地发现BPTES可以结合并抑制谷氨酰胺,有效地阻断肿瘤细胞的能量来源来饿死癌细胞,因此可有可能阻止肿瘤的生长。
研究人员表示下一步的研究工作还需考虑优化这一药物,提高其抑制肿瘤的效率并降低其副作用。

doi:10.1073/pnas.1116573109
PMC:
PMID:
Structural basis for the allosteric inhibitory mechanism of human kidney-type glutaminase (KGA) and its regulation by Raf-Mek-Erk signaling in cancer cell metabolism
K. Thangavelua, Catherine Qiurong Pana, Tobias Karlbergc, Ganapathy Balajid, Mahesh Uttamchandania,d,e, Valiyaveettil Sureshd, Herwig Schülerc, et al.
Besides thriving on altered glucose metabolism, cancer cells undergo glutaminolysis to meet their energy demands. As the first enzyme in catalyzing glutaminolysis, human kidney-type glutaminase isoform (KGA) is becoming an attractive target for small molecules such as BPTES [bis-2-(5 phenylacetamido-1, 2, 4-thiadiazol-2-yl) ethyl sulfide], although the regulatory mechanism of KGA remains unknown. On the basis of crystal structures, we reveal that BPTES binds to an allosteric pocket at the dimer interface of KGA, triggering a dramatic conformational change of the key loop (Glu312-Pro329) near the catalytic site and rendering it inactive. The binding mode of BPTES on the hydrophobic pocket explains its specificity to KGA. Interestingly, KGA activity in cells is stimulated by EGF, and KGA associates with all three kinase components of the Raf-1/Mek2/Erk signaling module. However, the enhanced activity is abrogated by kinase-dead, dominant negative mutants of Raf-1 (Raf-1-K375M) and Mek2 (Mek2-K101A), protein phosphatase PP2A, and Mek-inhibitor U0126, indicative of phosphorylation-dependent regulation. Furthermore, treating cells that coexpressed Mek2-K101A and KGA with suboptimal level of BPTES leads to synergistic inhibition on cell proliferation. Consequently, mutating the crucial hydrophobic residues at this key loop abrogates KGA activity and cell proliferation, despite the binding of constitutive active Mek2-S222/226D. These studies therefore offer insights into (i) allosteric inhibition of KGA by BPTES, revealing the dynamic nature of KGA's active and inhibitory sites, and (ii) cross-talk and regulation of KGA activities by EGF-mediated Raf-Mek-Erk signaling. These findings will help in the design of better inhibitors and strategies for the treatment of cancers addicted with glutamine metabolism.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PNAS#
25
#科学家发现#
22
#化合物#
37
#癌细胞#
28