Gastric Cancer:分泌型卷曲相关蛋白4(SFRP4)可促进胃癌的浸润并且是复发的早期预测指标
2020-12-05 MedSci原创 MedSci原创
胃癌(GC)是全球第五大最常见的癌症,也是癌症相关死亡的第三大原因,在缺乏有效筛查检查的国家中,GC患者通常在被诊断时就是晚期阶段,因此导致了很高的相关死亡率。
胃癌(GC)是全球第五大最常见的癌症,也是癌症相关死亡的第三大原因,在缺乏有效筛查检查的国家中,GC患者通常在被诊断时就是晚期阶段,因此导致了很高的相关死亡率。
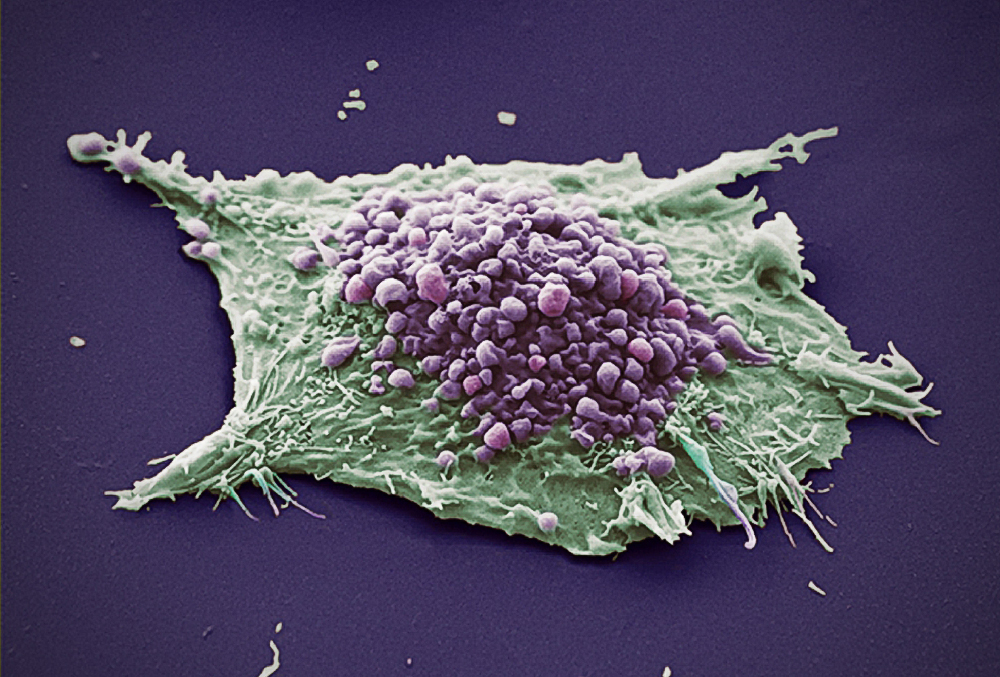
在大多数西方国家,总体5年生存率不到30%。虽然有各种各样的预测预后的工具,但是用于预测癌症复发的仍然是病理TNM分期系统,最近有研究表明与侵袭相关的关键基因的鉴定结果是用于预测GC预后的理想候选物。因此,这项研究旨在鉴定在癌症的最基本特征即入侵中起作用的基因,评估它们是否可以作为胃癌进展和复发的生物标志物。
研究人员使用K均值分析对来自cDNA表达阵列上的一组患者的数据进行了回顾性研究。这种基因组方法根据基因表达模式对数据进行分类,从而可以鉴定与GC入侵最相关的基因。研究人员从这项分析中评估了关键蛋白质在侵袭中的功能作用,并将其作为根治性切除术后复发的生物标志物。

最后研究人员发现分泌型卷曲相关蛋白4(SFRP4)的表达与胃癌的侵袭能力成正比。这项发现已在多个独立的数据集中得到验证,并且其在侵袭中的功能作用也已通过侵袭试验得以证实,胃癌患者行根治性切除后SFRP4血清水平的变化可以准确预测根治性治疗后疾病复发的风险。

这种简单的基于ELISA的测定方法可帮助预测治愈性胃癌手术后疾病的复发,而无需考虑辅助治疗的影响。本项研究的发现将有助于合理地制定癌症治疗方法和进行监测,以防止根治性切除术后患者治疗不足或过度。
原始出处:
Rita A. Busuttil. Et al. SFRP4 drives invasion in gastric cancer and is an early predictor of recurrence. Gastric Cancer.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#gastric#
42
#AST#
44
#GAS#
47
#分泌#
49
#预测指标#
56
学习
106