J Clin Oncol:阿美替尼有望成为EGFR突变的NSCLC患者的一线疗法
2022-05-27 MedSci原创 MedSci原创
阿美替尼有望成为EGFR突变的NSCLC患者的一线治疗选择
Aumolertinib(阿美替尼,原名Almonertinib;HS-10296)是一种新型三代表皮生长因子受体(EGFR)酪氨酸激酶抑制剂(TKI),可选择性、不可逆的抑制EGFR致敏性和T790M突变,在我国已获批上市。
近期发表在Journal of Clinical Oncology杂志上的AENEAS研究是一项双盲的3期临床试验,旨在比较阿美替尼与吉非替尼作为局部晚期或转移性EGFR突变的非小细胞肺癌(NSCLC)的一线治疗的疗效和安全性。
从我国的53个研究中心招募了组织学或细胞学明确诊断的局部晚期或转移性、携带EGFR突变(敏感性突变,如19外显子缺失和L858突变)的NSCLC患者,1:1随机分成两组,每日接受阿美替尼(110mg)或吉非替尼(250mg)治疗。主要终点是无进展生存期。
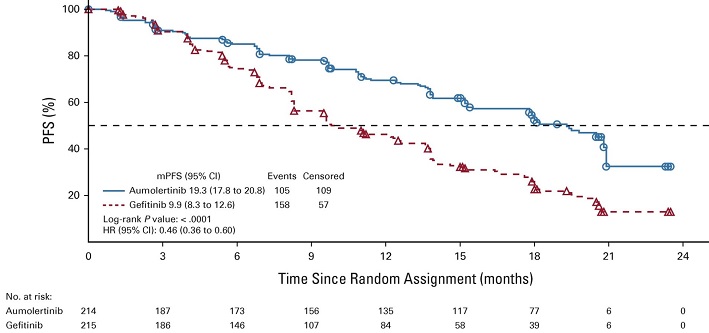
两组的无进展生存率
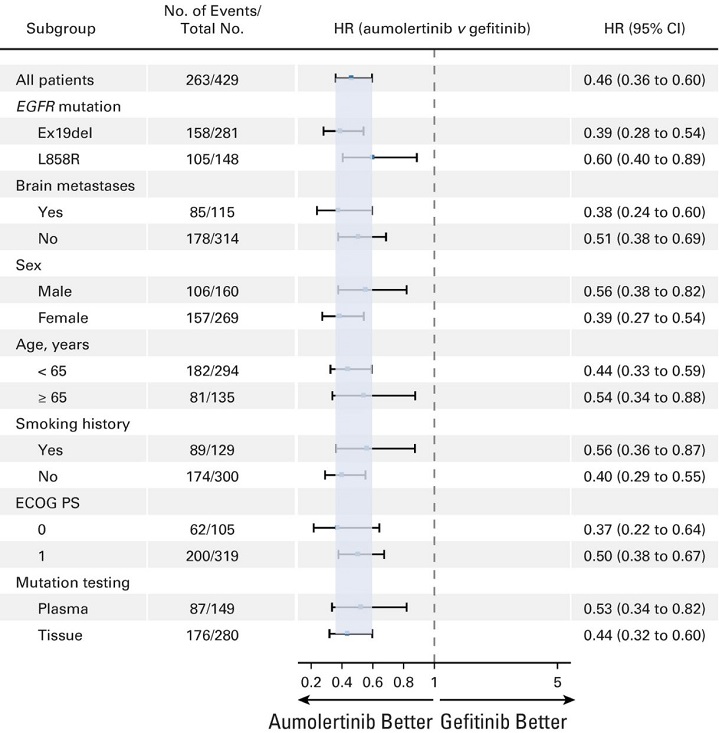
共招募了429位初治的局部晚期或转移性NSCLC患者。阿美替尼组的中位无进展生存期显著长于吉非替尼组(19.3个月 vs 9.9个月;风险比[HR] 0.46,95% CI 0.36-0.60, p<0.0001)。两组的客观缓解率和疾病控制率无明显差异(客观缓解率:73.8% vs 72.1%;疾病控制率:93.0% vs 96.7%)。阿美替尼组和吉非替尼组的中位缓解持续时间分别是18.1个月和8.3个月。
无进展生存率的亚组分析
阿美替尼组和吉非替尼组≥3级的不良事件的发生率分别是36.4%和35.8%。阿美替尼组所有级别的红疹和腹泻的发生率分别是23.4%和16.4%,在吉非替尼组这两种不良事件的发生率分别是41.4%和35.8%。
综上,阿美替尼是一种耐受性良好的三代表皮生长因子受体酪氨酸激酶抑制剂,有望成为EGFR突变的NSCLC患者的一线治疗选择。
原始出处:
Shun Lu, et al. AENEAS: A Randomized Phase III Trial of Aumolertinib Versus Gefitinib as First-Line Therapy for Locally Advanced or MetastaticNon–Small-Cell Lung Cancer With EGFR Exon 19 Deletion or L858R Mutations. Journal of Clinical Oncology. https://ascopubs.org/doi/full/10.1200/JCO.21.02641
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#SCLC患者#
56
#Oncol#
51
学习了
55
#NSCLC患者#
60
#GFR#
61