Circulation:A2R、PDE1C和TRPC3组成的多蛋白复合物参与调控心肌细胞的存活
2018-11-06 MedSci MedSci原创
cAMP在调节心肌细胞存活中起着关键作用。不同的cAMP信号通路作用明显或相反。Yishuai Zhang等研究人员既往发现通过环核苷酸磷酸二酯酶1C(PDE1C)激活cAMP水解可促进心肌细胞死亡/凋亡,但其分子机制尚不清楚。在本研究中,Yishuai Zhang等人尝试明确受PDE1C调控的特定cAMP信号通路,同时探究Ca2+/钙调蛋白激活PDE1C的机制。研究人员采用体外分离的小鼠成年心肌
研究人员采用体外分离的小鼠成年心肌细胞和阿霉素诱导的体内心脏毒性来研究心肌细胞的死亡/凋亡。同时采用多种药物激活剂/抑制剂以及基因编辑来控制目的蛋白的表达和活性。
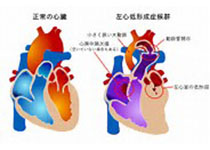
结果发现PDE1C抑制/缺陷对AngII(血管紧张素II)或阿霉素诱导的心肌细胞死亡/凋亡的保护作用是依赖于cAMP生成的腺苷A2受体(A2Rs),提示PDE1C的cAMP水解活性可选择性地调控心肌细胞中的A2R-cAMP信号。此外,研究人员还发现PDE1C激活对AngII介导的cAMP减少和心肌细胞死亡的影响依赖于瞬时受体电位(TRPC)通道,特别是TRPC3。研究人员还发现A2R刺激联合PDE1或TRPC抑制可协同保护心肌细胞存活。共染色和免疫沉淀研究表明PDE1C在质膜上的定位邻近A2R和TRPC3,特别是T小管。更重要的是,研究人员发现PDE1抑制剂IC86340或PDE1C敲除可缓解阿霉素诱导的小鼠心肌毒性和心肌功能异常,可保护作用又可被A2R拮抗剂消除。
总而言之,研究人员发现了一种新的多蛋白复合物,由A2R、PDE1C和TRPC3组成,其中PDE1C受TRPC3来源的Ca2+激活,进而拮抗A2R-cAMP信号、促进心肌细胞死亡/凋亡。上述分子或可成为保护心肌细胞存活的靶点。
Yishuai Zhang,et al.Multiprotein Complex With TRPC (Transient Receptor Potential-Canonical) Channel, PDE1C (Phosphodiesterase 1C), and A2R (Adenosine A2 Receptor) Plays a Critical Role in Regulating Cardiomyocyte cAMP and Survival.24 Jul 2018. Circulation. 2018;138:1988–2002
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PDE1C#
25
#TRPC3#
32
#复合物#
36
学习了
46