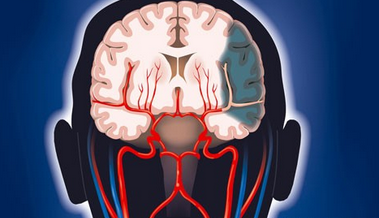
ISC 2018|大幅降低卒中风险——积极他汀治疗到底有多重要!
2018-01-27 沐雨 中国医学论坛报
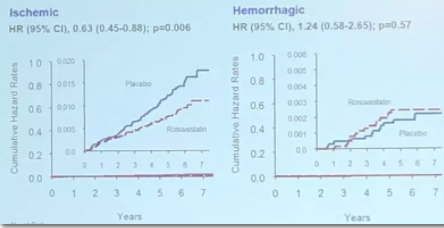
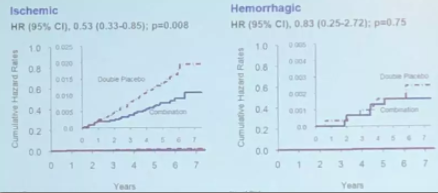
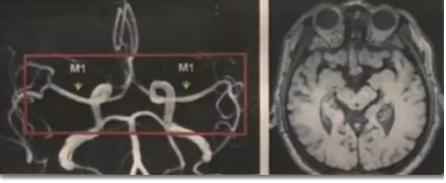
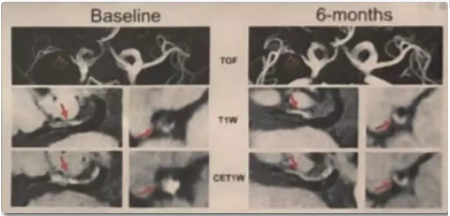
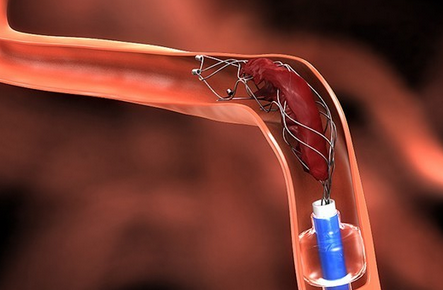
他汀是卒中预防的基石药物之一,有关瑞舒伐他汀预防卒中和稳定斑块的HOPE-3卒中亚组分析和REALM研究也在本次会议发布,其鼓舞人心的结果再次夯实了他汀在卒中防治中的重要地位。


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










非常好的文章.学习了
58
非常好的文章.学习了
48
学习..谢谢分享.
58
#卒中风险#
35
#ISC#
34
学习了分享了
52
学习.谢谢分享.
49
学习一下学习
32