哈佛专家撤回《细胞》“突破性” 研究论文
2016-12-31 孙学军 孙学军教授的博客
经过反复验证后,哈佛大学著名科学家Doug Melton(梅尔顿)撤回三年前发表在《细胞》杂志上的一篇论文(Cell:干细胞来源胰岛B细胞 未来或可根治糖尿病)(Cell:I型糖尿病疗法新突破)。 我当时在科学网上的介绍,甚至认为这属于2013年的突破性发现。http://blog.sciencenet.cn/blog-41174-684580.html 2013年,梅尔顿小组报道了一个新发现
梅斯医学编辑注:“自动撤稿”是科学家遵守科学规则的表现。研究成果出问题是常见的事情,只要符合国际惯例,正常撤回,这也是允许的。
下面是孙学军教授的博客文章:
经过反复验证后,哈佛大学著名科学家Doug Melton(梅尔顿)撤回三年前发表在《细胞》杂志上的一篇论文(Cell:干细胞来源胰岛B细胞 未来或可根治糖尿病)(Cell:I型糖尿病疗法新突破)。
我当时在科学网上的介绍,甚至认为这属于2013年的突破性发现。http://blog.sciencenet.cn/blog-41174-684580.html
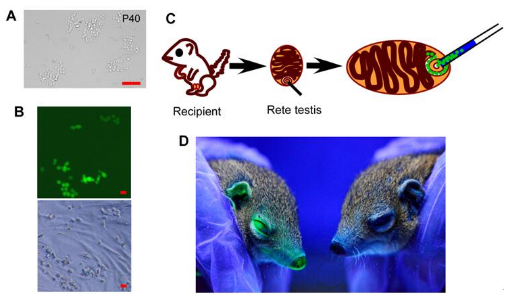
2013年,梅尔顿小组报道了一个新发现,提出肝脏能分泌一种刺激胰岛素分泌的激素betatrophin(胰岛营养因子),这样的激素显然能成为治疗糖尿病的潜在新方法。文章在《细胞》杂志发表后,哈佛大学著名学者,重要学术期刊,巨大的应用潜力,广泛的应用前景,这样的研究成果显然迅速成为了全世界科学界和媒体的关注热点。这样的新激素意味着可以让成千上万糖尿病患者摆脱长期注射胰岛素的困境。
2014年另一个独立的研究小组发现,梅尔顿小组报道的这个胰岛营养因子并不会影响胰岛素的分泌。梅尔顿小组随后对这种质疑进行了部分反驳。不过2016年,梅尔顿小组在Plos One发表文章承认了这种蛋白不具有刺激胰岛素分泌的功能。现在正式撤销2013年的《细胞》论文,在撤稿声明中明确提出当时的结论是错误的,缺乏足够的支持证据,这彻底埋葬了当时让人嫉妒的新发现。科学家这种勇于担当的态度是非常值得我们学习的。
梅尔顿告诉撤稿观察博客说撤回文章是为了避免造成混乱。betatrophin假说被推翻的过程说明科学家面对分歧时,应该如何一起工作,一起推动一个领域的进步。科学史表明,科学是曲折前进的。梅尔顿是干细胞研究的先驱,1990年代初,当他儿子被诊断出患有1型糖尿病,他决定致力于用干细胞制造胰岛素分泌β细胞,希望借此来治愈糖尿病。这一研究使他发现了betatrophin,在梅尔顿最初的论文中,他们发现给小鼠注射这种激素能让胰腺β细胞增长17倍。如果这样的作用也存在于人类,梅尔顿认为未来糖尿病患者可能只需要一年注射一次这样激素,而不必每天注射胰岛素。
但是此后一直无法重复这一结果,第一次研究只用了7个小鼠,当把实验动物扩大到先后5次52个动物,β细胞的数量开始大幅下降。Regeneron Pharmaceuticals公司的Viktoria Gusarova小组通过敲除和过表达betatrophin等方法,最终也无法证明这种蛋白刺激胰岛素细胞增生的能力。为了彻底验证这个假说,梅尔顿甚至招募了德克萨斯州贝勒医学院两个研究人员,三个小组开展动物盲法实验,结果仍然无法证明这个假说。最终只能放弃这一假说,将原始论文撤回。
PLoS One上反对的论文:
Cox AR, Barrandon O, Cai EP, Rios JS, Chavez J, Bonnyman CW, Lam CJ, Yi P, Melton DA, Kushner JA. Resolving Discrepant Findings on ANGPTL8 in β-Cell Proliferation: A Collaborative Approach to Resolving the Betatrophin Controversy. PLoS One. 2016 Jul 13;11(7):e0159276. doi: 10.1371/journal.pone.0159276.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












值得称道
78
值得尊敬
91
#哈佛#
36
文章不错,值得学习
82
好文章的好处
76