Science:研究提出更安全、更有效摧毁癌细胞的关键!
2017-10-07 枫丹白露 来宝网
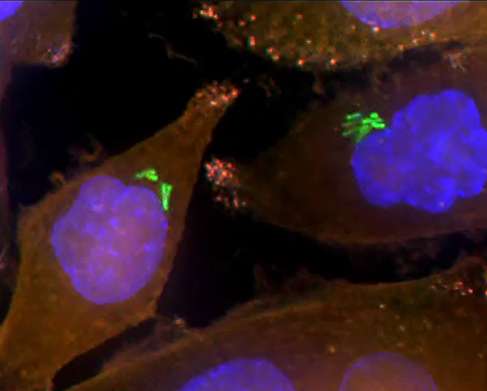
由国立卫生研究院科学家领导的国际小组首先发现一种新的方式,细胞可以修复称为DNA-蛋白质交联(DPC)的重要和危险类型的DNA损伤。研究人员发现,一种名为ZATT的蛋白质可以在另一种蛋白质TDP2的帮助下消除DPCs。由于DPCs在个体接受某些类型的癌症治疗时形成,因此了解TDP2和ZATT如何共同修复损伤可能会改善癌症患者的健康状况。研究结果发表在“科学”杂志上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#癌细胞#
27
#SCIE#
28
学习了.好文章
57
学习了学习了
56
henhao
64