BJU Int:西澳大利亚膀胱癌诊断和初始治疗的延期
2017-07-04 AlexYang MedSci原创
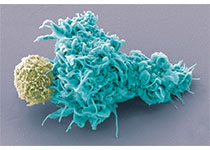
最近,有研究人员量化和检查了西澳大利亚膀胱癌病人诊断和初始治疗延期的原因。在2008年5月和2014年4月期间,研究人员对西澳大利亚的在一个公共的三级医院的一站式血尿诊所的所有参与者进行了回顾性检查。并且,研究人员对在该期间所有诊断为膀胱癌的病人进行了鉴定。另外,研究人员还回顾性的联系了这些病人和他们的GPs,并且邀请他们参与电话采访,同时从临床记录中搜集了额外的资料。还对患有可见血尿的病人的表现
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#初始治疗#
0
学习了谢谢分享!!
53
#澳大利亚#
24
学习了谢谢分享
2
值得推荐一下
66
学习并分享!!
53