Lancet:华法林抗凝监测过程中Fiix-凝血酶原时间更有效
2015-05-26 MedSci MedSci原创
背景 华法林在抗凝作用期间抗凝因子VII快速波动改变了国际标准化比值(INR),但对抗血栓作用贡献不大。该研究的目的是评估与标准PT-INR相比(包括凝血因子VII测量),仅由因素II和X(Fiix凝血酶原时间[Fiix-PT])影响的华法林抗凝稳定的非劣效性以及。 方法 该Fiix试验是一个单中心,双盲,前瞻性,非劣效
背景 华法林在抗凝作用期间抗凝因子VII快速波动改变了国际标准化比值(INR),但对抗血栓作用贡献不大。该研究的目的是评估与标准PT-INR相比(包括凝血因子VII测量),仅由因素II和X(Fiix凝血酶原时间[Fiix-PT])影响的华法林抗凝稳定的非劣效性以及。
方法 该Fiix试验是一个单中心,双盲,前瞻性,非劣效性,随机对照的临床试验。冰岛雷克雅未克,冰岛国立大学医院的门诊部里使用华法林达到2-3的INR目标并使用辅助软件确定抗凝剂量的成年人,符合本研究的纳入条件。研究人员排除了接受电击复转心律术的患者和护理之家的居民。患者通过组块随机被随机分配(1:1)到Fiix-PT监测组或PT监测组。基于各自的试验结果的双盲研究INR(R-INR)报告给计量人员。参与者通过一名研究护士在4周的时间间隔获取血栓或出血的信息,并与抗凝管理中心进行联系。主要疗效终点是一个客观诊断非致命性和致命性动脉或静脉血栓栓塞复合结果,包括心肌梗死和短暂性脑缺血发作,对所有符合条件的患者(意向性监测人群)进行评估。安全终点为大出血或其他临床相关的出血,在符合方案人群中进行评估。研究人员假设了一个3%的血栓栓塞年发病率和2.5%的非劣效性界点。
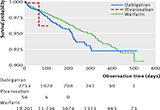
结果 在2012年3月1日到2014年2月28日之间,研究人员招收了1156例患者。由于各种原因每组排除四名患者后573例患者被分配到Fiix-PT组,575例患者被分配到PT-INR监测。中位随访时间为1.7年(IQR 1.1-1.9)。在1-720天之间,10例(1.2%每病人年)血栓栓塞事件发生在Fiix-PT组,19例(2.3%每病人年)发生在PT组(相对风险[RR] 0.52,95% Cl 0.25-1.13;Pnon-inferiority<0·0001)。Fiix组571例患者有17例(2.2%每病人年)发生大出血事件,PT组573例患者有20例发生大出血事件(2.5%每病人年;RR 0.85,0.45–1.61;Pnon-inferiority=0.0034)。抗凝治疗的稳定性随着在Fiix-PT组有所改善,这是和PT监测相比,由较少的测试,更少的剂量调整,增加的时间范围,较少的INR变化得到的结果。
结论 华法林的Fiix-PT监测提高了抗凝作用和剂量稳定性,在临床非劣于PT监测。这个试验的结果表明,维生素K拮抗剂治疗INR监测过程中可以由Fiix-PT替代,这和PT-INR监测相比,将得 到至少一个非劣性临床结果。
原始出处
Prof Páll T Onundarson, MDcorrespondence?email, Prof Charles W Francis, MD, Olafur S Indridason, MD, David O Arnar, MD, Prof Einar S Bjornsson, MD, Prof Magnus K Magnusson, MD, Sigurdur J Juliusson, BS, Hulda M Jensdottir, BS, Brynjar Vidarsson, MD, Petur S Gunnarsson, PharmD, Sigrun H Lund, PhD, Brynja R Gudmundsdottir, MS?,Fiix-prothrombin time versus standard prothrombin time for monitoring of warfarin anticoagulation.Lancet,2015.5.25
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Lancet#
0
看看
126
看看
158
#凝血酶原#
40
#华法林抗凝#
40