Eur Heart J:胺碘酮不影响依度沙班安全有效性
2015-05-25 张旭栋译 MedSci原创
University Heart Center Zurich的Steffel, J等人研究了胺碘酮对于依度沙班安全有效率的研究,其研究成果发表在5月份European heart journal期刊上。 背景: 在ENGAGE AF-TIMI48试验中,高剂量依度沙班(HDE)缺血性中风的发生率与华法林相似,而低剂量(LDE)组中的发生率却相对较高。胺碘酮可以通过抑制P-糖蛋白从而增加依度沙班
University Heart Center Zurich的Steffel, J等人研究了胺碘酮对于依度沙班安全有效率的研究,其研究成果发表在5月份European heart journal期刊上。
背景:
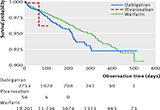
在ENGAGE AF-TIMI48试验中,高剂量依度沙班(HDE)缺血性中风的发生率与华法林相似,而低剂量(LDE)组中的发生率却相对较高。胺碘酮可以通过抑制P-糖蛋白从而增加依度沙班血浆水平。本研究旨在探索胺碘酮对依度沙班相对有效性和安全性的疗效。
方法和结果:
2492例(占总比例对11.8%)患者接受胺碘酮治疗。与未服用胺碘酮的患者相比,LDE组中风或全身性栓塞的主要疗效终点事件发生率显著降低(服用华法林并服用胺碘酮的患者风险比[HR]0.60,95%置信区间0.36-0.99;服用华法林并未服用胺碘酮的患者HR1.20,95%可信区间1.03-1.40,P<0.01)。患者随机接受HDE组,相同的比较并没有发现存在显著的交互式疗效(HR:0.73,95%可信区间0.46-1.17比HR:0.89,95%可信区间0.75-1.05,P=0.446)。独立使用胺碘酮的患者,与服用华法林组相比,LDE组主要出血事件(HR:0.35,95%可信区间0.21-0.59比HR:0.53,95%可信区间0.46-0.61,P=0.131)和HDE组主要出血事件(HR:0.94,95%可信区间0.65-1.38比HR:0.79,95%可信区间0.69-0.90,P=0.392)。
结局:
服用华法林患者中,与未同时使用胺碘酮的患者相比,同时使用胺碘酮的患者缺血事件发生显著降低。 与此相反,胺碘酮对HDE的相对有效性和安全性没有影响。
原文出处:
Steffel J, Giugliano RP, Braunwald E, et al. Edoxaban vs. warfarin in patients with atrial fibrillation on amiodarone: a subgroup analysis of the ENGAGE AF-TIMI 48 trial. European heart journal. 2015.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#胺碘酮#
35
#ART#
0
#HEART#
25
看看
98