AHA 2013:缺血性二尖瓣返流—修复瓣膜与置换瓣膜哪种手段更具优势?
2013-11-20 佚名 丁香园
2013年11月18日,美国心脏协会(AHA)2013科学年会公布的最新临床试验显示,严重缺血性二尖瓣返流(SMR)患者接受二尖瓣修复或置换术后的心脏功能和生存率相似,且后者的返流复发率更低。 缺血性二尖瓣返流是心肌梗死的常见并发症,返流严重者可出现包括心力衰竭或心律失常等症状。当前指南推荐可以选择二尖瓣修复术或二尖瓣置换术,但尚无证据证明哪种方式效果更佳,两种方法各
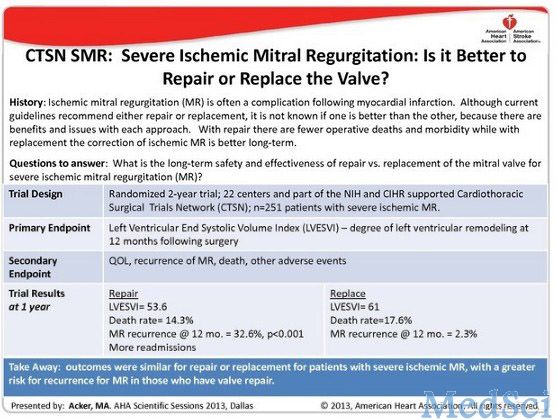
2013年11月18日,美国心脏协会(AHA)2013科学年会公布的最新临床试验显示,严重缺血性二尖瓣返流(SMR)患者接受二尖瓣修复或置换术后的心脏功能和生存率相似,且后者的返流复发率更低。
缺血性二尖瓣返流是心肌梗死的常见并发症,返流严重者可出现包括心力衰竭或心律失常等症状。当前指南推荐可以选择二尖瓣修复术或二尖瓣置换术,但尚无证据证明哪种方式效果更佳,两种方法各有利弊。
心胸外科临床研究网络(CTSN)严重二尖瓣关闭不全(SMR)随机试验是宾夕法尼亚大学佩雷尔曼学院医学院进行的一项为期2年的临床研究。该研究调查了美国22个临床中心251例严重缺血性二尖瓣关闭不全患者,比较125例接受瓣膜置换术患者和126例瓣膜修补患者的预后。
研究发现,1年后修复组的死亡率为14.3%,置换组为17.6%.修复组和置换组左心室收缩末期容积指数(LESVI)分别为53.6 ml/m2和61 ml/m2.两组间严重不良事件、功能状态、生活质量和再住院率无显著差异。术后12个月内二尖瓣返流复发率,修复组为32.6%,置换组仅为2.3%.修复组有3例患者需再次手术,置换组则无。
该研究负责人Michael Acker博士表示,“许多心脏外科医生和心内科医生都有一个明显偏见,认为二尖瓣修复术总是优于置换术,即使对严重二尖瓣返流的患者亦是如此。我们的研究结果则推翻了这样的观点,尽管修复术和置换术的临床结果相似,但二尖瓣修复术的返流复发率更高。对于严重二尖瓣返流的患者来说,二尖瓣置换术或许更胜一筹。
缺血性二尖瓣返流:修复瓣膜与置换瓣膜哪种手段更具优势?
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#缺血性#
33
#置换#
40
#AHA#
40
#二尖瓣返流#
36
#二尖瓣#
35
#瓣膜#
27