Circulation:冠心病的另一种新的诊断试验——冠状动脉CT血管造影的非侵入性血流储备分数
2017-07-31 MedSci MedSci原创
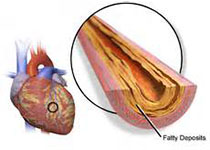
尽管局部缺血评估具有临床重要性,但在浸润性心导管术中,获得性流量储备(FFR)仍然具有价值。虽然形态学与生理学之间有明显的联系,但仍然存在显著的差异。来源于冠状动脉CT血管造影的血流储备分数(FFRCT)是一种通过将形态学信息转化为血流动力学数据的方法来量化冠状动脉狭窄的血流动力学意义的一种新方法。
尽管局部缺血评估具有临床重要性,但在浸润性心导管术中,获得性流量储备(FFR)仍然具有价值。虽然形态学与生理学之间有明显的联系,但仍然存在显著的差异。来源于冠状动脉CT血管造影的血流储备分数(FFRCT)是一种通过将形态学信息转化为血流动力学数据的方法来量化冠状动脉狭窄的血流动力学意义的一种新方法。与冠状动脉CT血管造影术相比,FFRCT了提高诊断性能,其具有侵入性的FFR参考标准。这项技术的潜在好处是可以安全地推迟无指示的导管插管以及降低医疗费用,并表明这项技术可以改善冠心病治疗。研究人员总结了FFRCT的科学依据和临床试验证据,为临床应用提供了例证,探讨了潜在的局限性,并为今后的研究提供了思路。在不需要侵入性手术的前提下,FFRCT使得特殊病变局部缺血的计算成为可能。之前的多中心试验的结果一致显示cCTA提高了诊断准确性。此外,在临床研究和临床实践中,FFRCT已经被证明能够安全地延迟高达60%的诊断心导管检查程序。由此可见,与通常的护理相比,FFRCT在成本效益和症状缓解方面存在潜在益处。将FFRCT引入临床实践可能会改变CAD患者的传统治疗方法。原始出处:Hiromasa Ot
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#诊断试验#
55
#非侵入性#
0
#冠状动脉CT血管造影#
47
#侵入性#
48
#冠状动脉CT#
49
#造影#
40
学习一下知识
73