ADCFNE:动脉导管未闭早期治疗的相关研究
2021-09-18 从医路漫漫 MedSci原创
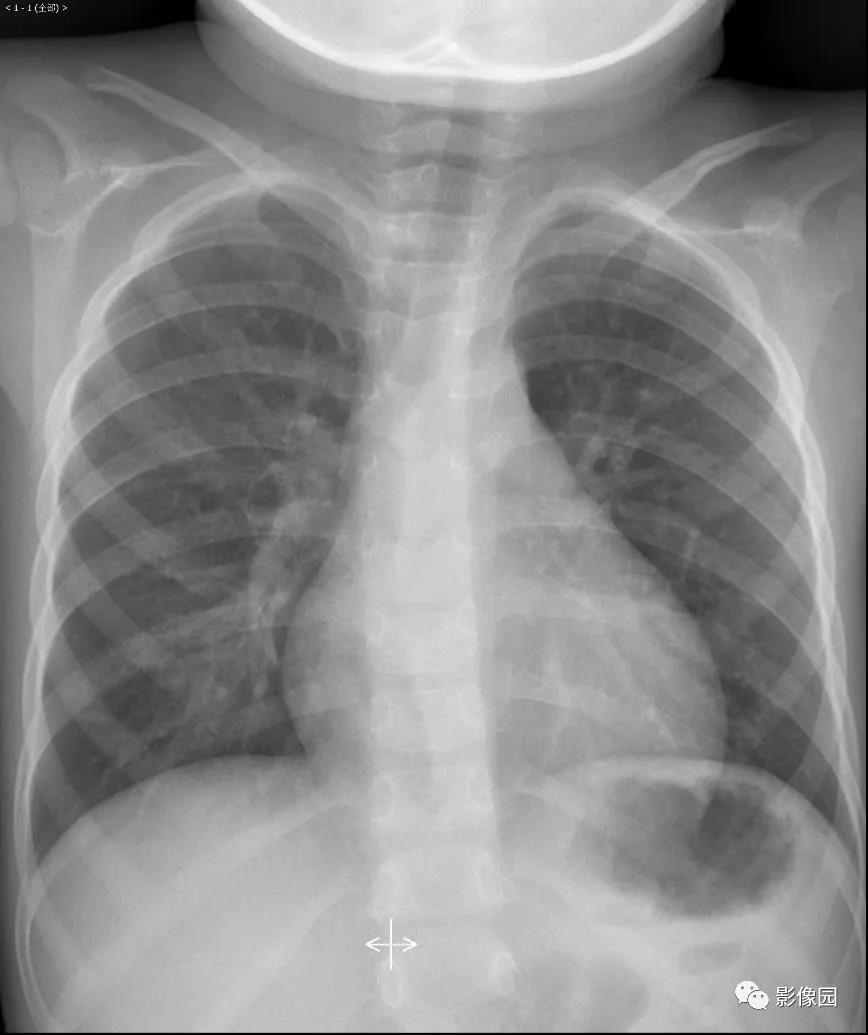
早期或预防性治疗动脉导管未闭(PDA)可降低脑室周围/脑室内出血(PIVH)和肺出血(PH)的发生率,并减少随后进行内科或外科封堵的需要。
早期或预防性治疗动脉导管未闭(PDA)可降低脑室周围/脑室内出血(PIVH)和肺出血(PH)的发生率,并减少随后进行内科或外科封堵的需要。尽管有这些明显的短期益处,但这并没有转化为改善幸存婴儿的结果,而且这种做法还没有被广泛采用。临床医生似乎不愿意让婴儿接受这种治疗,因为这种治疗对一些婴儿有很大的好处,但也有潜在的危害,包括肾脏损害、胃肠道损伤、液体潴留、支气管肺发育不良(BPD)和短暂性脑血管限制的风险。
在出生后的早期,极早产儿导管收缩的特点是差异很大,那些收缩不良的婴儿患PIVH、PH的风险较高,随后需要PDA治疗。如果早期预防性治疗可以只针对那些PDA狭窄程度较差的患者,那么好处可能会最大化,潜在的危害可能会最小化。我们假设,对29周之前出生的婴儿进行早期超声靶向PDA治疗,可以降低死亡率和异常的颅脑超声检查结果,以及随后需要内科或外科闭合PDA,而不会增加短期的不良反应。
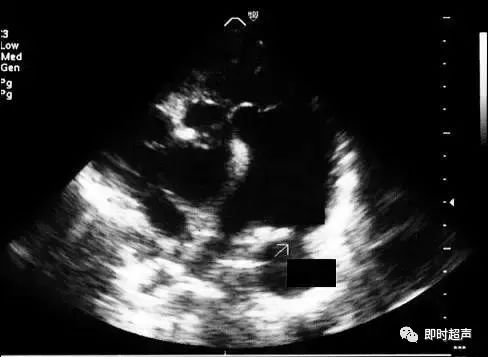
目的:动脉导管未闭(PDA)可能与损伤有关。早期对大的PDA进行心脏超声靶向治疗可减少不良结果,并需要在不增加不良反应的情况下进行后期的PDA闭合。
方法:多中心、双盲、随机对照试验。对出生小于29周的婴儿进行大PDA筛查,并在12小时前接受吲哚美辛或安慰剂治疗。
结果:由于缺乏吲哚美辛,试验提前终止了登记。12h前筛查164例符合条件的婴儿,在92例创面大PDA婴儿中,44例随机使用消炎美辛,48例使用安慰剂。两组之间的主要结果没有差异。接受早期吲哚美辛治疗的婴儿早期肺出血(PH)明显减少(2% vs 21%),脑室周围/脑室出血(PIVH)减少(4.5% vs 12.5%),随后接受PDA开放标签治疗的可能性更小(20% vs 40%)。72例创面小的PDA非随机婴儿肺出血风险低,自发性PDA闭合率为80%。

表1 创面大的动脉导管未闭(PDA)婴儿随机服用消炎美辛或安慰剂的结果

表2 创面大的动脉导管未闭(PDA)婴儿随机使用消炎美辛或安慰剂的次要结局
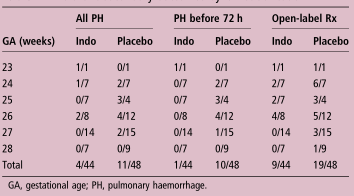
表3 GA分层相关次级结果;GA,胎龄;PH值、肺出血。
结论:早期心脏超声靶向治疗创面大的PDA是可行和安全的,可减少早期肺出血和后期药物治疗,但对死亡或异常颅超的主要结果没有影响。
原文出处
Kluckow M, Jeffery M, Gill A, Evans N,A randomised placebo-controlled trial of early treatment of the patent ductus arteriosus.Arch Dis Child Fetal Neonatal Ed 2014 Mar;99(2)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#DCF#
51
#早期治疗#
37
#相关研究#
45
#动脉导管未闭#
35